Laparoscopic management of giant adrenal cyst: a case report
Highlight box
Key findings
• A case of a patient with a giant adrenal cyst is reported, along with a detailed description of the laparoscopic management of the cyst. A video showcasing the technique employed is included. The patient exhibited a satisfactory evolution without complications.
What is known and what is new?
• Adrenal cysts are rare pathological entities (<1% of all adrenal lesions). The average size of adrenal cysts reported in the literature is 5 cm. There is no consensus regarding the treatment of such cysts.
• In patients with giant adrenal cysts (>10 cm), a proper diagnostic and therapeutic approach can lead to its resolution through Minimally Invasive Surgery.
What is the implication, and what should change now?
• Adrenal cysts larger than 10 cm can be safely resected through laparoscopic surgery for the patient’s benefit.
Introduction
Background
The first adrenal cyst was described in 1670 (1). Adrenal cyst are rare lesions that normally are incidentally discovered on imaging examinations for another cause with very low prevalence <1% among all adrenal lesions.
Rationale and knowledge gap
Adrenal cysts often remain asymptomatic or with nonspecific symptoms, which contributes to the underdiagnosis of these lesions. Most cases are incidentally diagnosed (88%), with an average size of 48 mm upon diagnosis (2). Currently, there is no consensus regarding the management of such lesions due to their rarity.
Objective
The purpose of this case is to review the management and surgical approach of giant adrenal cyst. We present this case in accordance with the CARE reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-23-12/rc).
Case presentation
A 47-year-old female patient from Campeche, Mexico, is presented to the general surgery service. The patient denies allergies, tobacco, and alcohol consumption, with a surgical history of open cholecystectomy and lateral internal sphincterotomy.
In May 2021, she started with moderate and persistent pain in the left lumbar region, so an ultrasound was performed, which reported a left adrenal tumor. She was transfer to a tertiary health care center.
Physical exploration
The patient presented with vital signs within normal range, with a body mass index of 33.7 kg/m2 (Grade I obesity). Abdomen with a palpable tumor on the left flank of approximately 10 cm × 10 cm, poorly defined borders, fixed to deep planes, with pain on palpation 4/10 on the Visual Analogue Scale of pain. Laboratory test with leukocytes of 4.07×103/L [reference value (4.6–10.4)×103/L], creatinine 0.74 mg/dL (reference value 0.50–1.20 mg/dL), dehydroepiandrosterone 73.7 mcg/dL (reference value 19–231 mcg/dL), serum metanephrines 134.6 pg/mL (reference value 33–190 pg/mL), morning cortisol 11.1 mcg/dL (reference value 3.7–19.4 mcg/dL), evening cortisol 3.35 mcg/dL (reference value 2.9–17.3 mcg/dL), testosterone 0.20 ng/mL (reference value 0.20–0.81 ng/mL). Serum electrolytes and coagulation times within normal parameters.
Abdominal computed tomography (CT) scan with intravenous contrast was performed, which reported a single and simple cystic lesion dependent on the left adrenal gland with thin walls, homogeneous, with a density of 11 Hounsfield units, measuring 152 mm × 145 mm × 122 mm, which generated extrinsic compression to adjacent structures (Figure 1).

Endocrinologic assessment ruled out a functional tumor—adrenal mass.
Preoperative evaluation by Internal Medicine and anesthesiology with Goldman risk index class I and American Society of Anesthesiologists score class II.
Surgical procedure
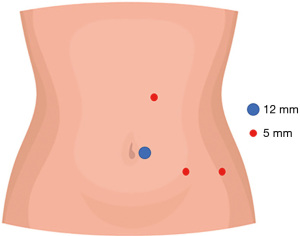
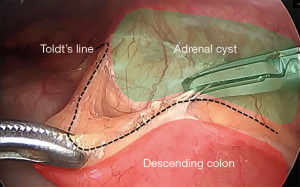
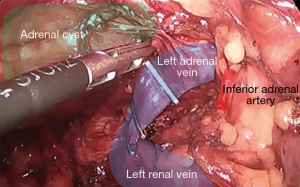
Prophylactic antibiotic according to local guidelines. With the patient under balanced general anesthesia, in a right lateral decubitus position, a 12-mm left paraumbilical trocar was placed. Under direct vision, three 5-mm trocars are placed, two in the left flank and one in the left subcostal region (Video 1, Figure 2). A Mattox maneuver was performed from the rectosigmoid junction to the splenic flexure, with bipolar energy (Figure 3), exposing the 15 cm × 14 cm × 11 cm adrenal cyst firmly adherent to the left adrenal gland. Adhesions were released from the cyst to the abdominal wall, ipsilateral kidney, tail of the pancreas, stomach, and spleen. Control of the adrenal vein was performed with metallic clips and control of the adrenal artery with bipolar energy (Figure 4). Before extraction, the cyst is drained obtaining approximately 1,200 mL of a viscous yellow liquid. The piece is removed in a bag through the paraumbilical 12 mm trocar. The procedure was performed under 245 minutes with bleeding of 30 mL.
Postoperative evolution and follow-up
Multimodal analgesia and antibiotic prophylaxis were continued for 24 hours after surgery. She tolerated orally with liquids 4 hours after surgery and progressed to a soft diet the next day. The patient was discharged 24 hours after the procedure with a double non-steroidal anti-inflammatory drug (NSAID). A follow up visit was scheduled at 7 and 21 days postoperative, without any complaints.
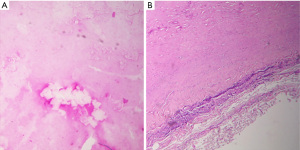
Histopathology
Pseudocyst wall with chronic reparative process and fibrosis, dystrophic calcification, and adrenal gland without significant histological alterations are reported. The cyst contained a yellowish fluid corresponding to an acellular proteinaceous liquid. Histopathological images appear in Figures 5,6.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
Adrenal cysts represent a rare disease, with a reported incidence of 0.06–0.18%. Generally, these cysts present in the fourth/fifth decades of life (3-5). The clinical presentation can vary from being asymptomatic, subclinical symptoms or presenting complications such as bleeding, infection, or rupture. In the case of giant cysts (>10 cm), vague symptoms may occur due to mass effect towards neighboring organs (6).
Benign adrenal cysts are classified into four categories: vascular (45%), pseudocysts (39%), epithelial (9%), and parasitic (7%). Furthermore, adrenal cysts can be classified as functioning and non-functioning (3,7,8).
The differential diagnosis of retroperitoneal cysts may include lesions of neoplastic origin such as cystic lymphangioma, mucinous cystadenoma, cystic teratoma, cystic mesothelioma, Müllerian cyst, epidermoid cyst, bronchogenic cyst, cystic change in solid neoplasms, pseudomyxoma retroperitoneal and lesions of non-neoplastic origin such as pancreatic pseudocyst, non-pancreatic pseudocyst, lymphocele, urinoma, hematoma (5). Adrenal hydatid cysts are infrequent (<1% of echinococcosis cases) and typically exhibit distinctive features on computed tomography, such as simple cysts with a double wall, multilocular cysts, the presence of the daughter cyst sign, calcifications in septa or capsule, and membrane detachment (9,10). The case presented did not show any past medical history or clinical manifestations, nor did the imaging data indicate any evidence suggestive of an Echinococcus granulosus infection.
CT scan is the study of choice for the approach to adrenal masses with a sensitivity of 85–95%. The characteristic findings of adrenal cysts are thin non-enhancing walls and fluid density content; higher density within the cyst suggests a complication such as hemorrhage (11).
The treatment depends on whether it is functional or not, the size and the symptoms. Therefore, the work-up should include: 24-h urinary metanephrines [or vanillylmandelic acid (VMA)], 17-hydroxycorticosteroids and 17-ketosteroids measurements. The low-dose dexamethasone test can evaluate the suppression rate of urinary steroids (11). The measurement of the aldosterone/renin ratio is warranted solely in patients exhibiting associated hypertension and/or hypokalemia; hence, there was no necessity to perform this assessment in the present case (12-14).
Indicators pointing towards a malignant adrenal tumor encompass age younger than 40 years, rapid symptom development, excessive production of adrenocortical hormones, and tomographic findings suggestive of malignancy (density >10–21 HU, heterogeneous appearance, size >4 cm) (15,16). In contrast, the patient under examination exhibited no abnormalities in adrenal hormones, and while the tumor size exceeded 4 cm, all other clinical, biochemical, and imaging characteristics pointed towards a benign tumor. When malignancy is suspected (which occurs in 7% of cases and it is the second most aggressive endocrine malignant disease after anaplastic thyroid carcinoma) the recommendation is to perform a surgical exploration (8). Other indications for surgery include cysts >4 cm, functional, parasitic, complicated cysts and those who present symptoms (11).
In cases of patients with adrenal tumors exhibiting borderline features on imaging studies, functional imaging modalities like single photon emission tomography or positron emission tomography can be employed to assess laterality (unilateral or bilateral tumors) in functioning masses, as well as to differentiate between benign nodules and malignant adrenal disease in non-functioning tumors (17).
Although minimally invasive adrenalectomy serves as the gold standard for managing most benign adrenal lesions, particularly tumors with a diameter of up to 6 cm, the definitive approach should be selected based on diagnostic suspicion, cyst characteristics, and the surgeon’s experience. In instances where malignancy is suspected, open surgery represents the standard treatment, although tumors smaller than 6 cm lacking evidence of local invasion can be effectively resected laparoscopically, provided the procedure is performed by an experienced surgeon in this field (15). In the case of hydatid cysts, both laparoscopic and open surgical methods can be considered, with careful consideration of the risk of cyst rupture and the potential consequences of anaphylactic shock and cyst dissemination. In situations where surgical intervention is not feasible, the PAIR method (Puncture, Aspiration, Injection, and Re-aspiration) can be regarded as an alternative option (18). This technique entails image-guided puncture and aspiration of the cyst, followed by irrigation with a hypertonic solution or alcohol, and re-aspiration of the cyst’s contents.
Strengths and limitations
The laparoscopic approach provides reduced surgical trauma, shorter recovery time, and improved aesthetic outcomes. Decreasing surgical trauma facilitates an early return to daily activities. The disadvantage of the minimally invasive approach in giant cysts is associated with the reduction of available space in the abdominal cavity due to the mass effect. This can be corrected through proper patient positioning and the appropriate distribution of trocars, enabling adequate manipulation of the cyst.
Comparison with similar researches
Therapeutic modalities available are open surgery with cyst enucleation (recommended for cysts densely adherent to adjacent organs), open surgery with en bloc adrenalectomy with cyst resection in cases of malignancy, or laparoscopic surgery with cyst decortication and partial or total adrenalectomy.
Robot-assisted approaches present a potential alternative for the management of adrenal cysts. Comparable outcomes have been documented when comparing laparoscopic adrenalectomy with robot-assisted adrenalectomy in terms of postoperative hospitalization, intraoperative complications, postoperative complications within 30 days, and cost-effectiveness. Substantial benefits have been noted in high-volume medical centers, specifically among patients with functional tumors and/or those presenting tumors larger than 6 cm (19,20).
Laparoscopic partial adrenalectomy stands as the preferred procedure for the resection of adrenal cysts, since the adrenal gland is preserved (7,11). Nevertheless, a considerable number of giant adrenal cyst cases continue to be managed through open surgical procedures, even in specialized referral centers (4-6,8,11). The presented case exemplifies the viability of employing a laparoscopic approach for managing such lesions, complemented by a visual elucidation of the procedure.
Explanations of findings
In this patient, the dimensions of the cyst caused displacement of intra-abdominal organs. The appropriate positioning of the patient and working ports allowed for adequate exposure of the cyst boundaries. The lateral decubitus position provided gravitational traction, facilitating the exposure of dissection planes, and separating the organs adhered to the cyst. Once the lesion was dissected, controlled aspiration of its contents allowed for proper extraction without the need for additional incisions. The patient’s prompt and satisfactory recovery is attributed to the utilization of a minimally invasive approach, which avoided the need for a large incision that would have been necessary for adequate cyst exposure in an open surgery.
Implications and actions needed
The description of cases involving successfully treated giant adrenal cysts using minimally invasive surgery promotes the application of this approach in these patients. The necessity for conducting studies that compare the outcomes of open and laparoscopic approaches is evident. However, conducting such studies is challenging due to the limited number of patients with this disease.
Conclusions
Adrenal cysts are uncommon lesions, with giant adrenal cysts being even rarer. Despite the most reported cases of giant adrenal cysts have been treated using open approaches, the appropriate diagnostic and therapeutic approach render laparoscopic resection safe and effective in these patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-23-12/rc
Peer Review File: Available at https://ls.amegroups.com/article/view/10.21037/ls-23-12/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-23-12/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Song JH, Chaudhry FS, Mayo-Smith WW. The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol 2008;190:1163-8. [Crossref] [PubMed]
- Dogra P, Rivera M, McKenzie TJ, et al. Clinical course and imaging characteristics of benign adrenal cysts: a single-center study of 92 patients. Eur J Endocrinol 2022;187:429-37. [Crossref] [PubMed]
- Bellantone R, Ferrante A, Raffaelli M, et al. Adrenal cystic lesions: report of 12 surgically treated cases and review of the literature. J Endocrinol Invest 1998;21:109-14. [Crossref] [PubMed]
- Cavallaro G, Crocetti D, Paliotta A, et al. Cystic adrenal lesions: clinical and surgical management. The experience of a referral centre. Int J Surg 2015;13:23-6. [Crossref] [PubMed]
- Chodisetti S, Boddepalli Y, Kota M. Giant adrenal cyst displacing the right kidney. Indian J Urol 2016;32:81-2. [Crossref] [PubMed]
- Chaabouni A, Samet A, Harbi H, et al. A case of a giant adrenal cyst. Urol Case Rep 2021;38:101725. [Crossref] [PubMed]
- Amarillo HA, Bruzoni M, Loto M, et al. Hemorrhagic adrenal pseudocyst: laparoscopic treatment. Surg Endosc 2004;18:1539. [Crossref] [PubMed]
- Chatzoulis G, Passos I, Bakaloudi DR, et al. Giant nonfunctioning adrenal tumors: two case reports and review of the literature. J Med Case Rep 2018;12:335. [Crossref] [PubMed]
- Yu XK, Zhang L, Ma WJ, et al. An Overview of Hepatic Echinococcosis and the Characteristic CT and MRI Imaging Manifestations. Infect Drug Resist 2021;14:4447-55. [Crossref] [PubMed]
- Staouni IB, Bouardi NE, Ferhi M, et al. Primary hydatid cyst of adrenal gland: Case report. Radiol Case Rep 2022;17:3188-90. [Crossref] [PubMed]
- Sioka E, Symeonidis D, Chatzinikolaou I, et al. A giant adrenal cyst difficult to diagnose except by surgery. Int J Surg Case Rep 2011;2:232-4. [Crossref] [PubMed]
- Lee JM, Kim MK, Ko SH, et al. Clinical Guidelines for the Management of Adrenal Incidentaloma. Endocrinol Metab (Seoul) 2017;32:200-18. [Crossref] [PubMed]
- Fassnacht M, Arlt W, Bancos I, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 2016;175:G1-G34. [Crossref] [PubMed]
- Funder JW, Carey RM, Mantero F, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2016;101:1889-916. [Crossref] [PubMed]
- Fassnacht M, Dekkers OM, Else T, et al. European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 2018;179:G1-G46. [Crossref] [PubMed]
- Petersenn S, Richter PA, Broemel T, et al. Computed tomography criteria for discrimination of adrenal adenomas and adrenocortical carcinomas: analysis of the German ACC registry. Eur J Endocrinol 2015;172:415-22. [Crossref] [PubMed]
- Lorusso M, Rufini V, DE, Crea C, et al. Integration of molecular imaging in the personalized approach of patients with adrenal masses. Q J Nucl Med Mol Imaging 2022;66:104-15. [Crossref] [PubMed]
- Abbasi B, Akhavan R, Ghamari Khameneh A, et al. Computed tomography and magnetic resonance imaging of hydatid disease: A pictorial review of uncommon imaging presentations. Heliyon 2021;7:e07086. [Crossref] [PubMed]
- De Crea C, Pennestrì F, Voloudakis N, et al. Robot-assisted vs laparoscopic lateral transabdominal adrenalectomy: a propensity score matching analysis. Surg Endosc 2022;36:8619-29. [Crossref] [PubMed]
- De Crea C, Arcuri G, Pennestrì F, et al. Robotic adrenalectomy: evaluation of cost-effectiveness. Gland Surg 2020;9:831-9. [Crossref] [PubMed]
Cite this article as: Navarro Castañeda CA, Romero Sanchez JA, Garcia Cordova CE, Farell Rivas J, Torres Iparrea G, Valdez Mendieta HY. Laparoscopic management of giant adrenal cyst: a case report. Laparosc Surg 2023;7:16.