Candy cane syndrome related with weight loss failure after laparoscopic gastric bypass: a case report
Highlight box
Key findings
• This case presents a patient with marginal weight loss after laparoscopic gastric bypass as the main complaint leading to the identification of a large blind alimentary limb.
What is known and what is new?
• Candy Cane syndrome is a rare clinical entity described in patients after laparoscopic gastric bypass.
• A large “Candy Cane” in a patient with gastric bypass could be an exceptional cause of poor postoperative weight loss.
What is the implication, and what should change now?
• Asses for the presence of a long blind limb “Candy Cane” during upper endoscopy and oral contrast fluoroscopy in patients with suboptimal postoperative weight loss.
• Surgical revision could reverse suboptimal weight loss in these patients
Introduction
Obesity has become a major public health concern during the last decades. Globally, close to 1.9 billion people are considered overweight and up to 650 million more are morbidly obese (1). Bariatric surgery, a readily available treatment in most countries, has become the standard of treatment for this aggravating disease being laparoscopic gastric bypass (LGBP), one of the most performed bariatric procedures around the world (2).
Candy cane syndrome (CCS) has been described as an unusual complication of LGBP. It is related to an excessively long blind end of the alimentary limb just distal to the gastro-jejunal anastomosis which can retain undigested food remains (3). CCS is classically considered a rule out diagnosis and is often accompanied with non-specific symptoms such as abdominal pain, dysphagia, regurgitation, nausea and vomiting (4). The pathophysiology of the symptoms presumably derives from an increased intraluminal pressure of the blind end of the alimentary limb. The increment of pressures results in structural changes (increasing size) of the grastro-jejunal anastomosis losing an important restrictive component for weight loss after LGBP.
We present the case of a patient with CCS. We present this case in accordance with the CARE reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-23-5/rc).
Case presentation
We present the case of a 34-year-old lady with a Body Mass Index (BMI) of 46.7 kg/m2 (132 kg). She had relevant comorbidities associated with obesity including dyslipidemia, moderate obstructive sleep apnea, hypothyroidism and insulin resistance. The patient was evaluated in an outside hospital as a candidate for bariatric surgery. Ultimately a LGBP was performed in July 2019 without any postoperative immediate complications. She was discharged and unfortunately did not take a regular post operative clinical follow up.
The patient presented to our institution 3 years after the primary procedure with a maximal total weight loss of only 8 kg (BMI of 44.8/12.7% excess weight loss) obtained 3 months after surgery. Interestingly, the patient reported that weight loss was very difficult to maintain despite her adherence to a regular exercise and dietary plan. She also complained from occasional epigastric pain accompanied with a bulging sensation around the upper abdomen after meals. She remarkably states that was able to eat meals in big quantities without any feeling of satiety. She reported unpleasant feelings regarding her suboptimal weight loss after surgery, with low motivation and her expectations completely unfulfilled. Thus, a complete workup was performed in order to establish the cause of the unsuccessful weight loss in this patient. Additionally, a multidisciplinary team evaluated the patient and ruled out alternative differential diagnosis or coexisting eating disorders.
The outside hospital operatory report was obtained and revealed a standard configuration of the LGBP in a classic Roux in Y fashion with an antecolic alimentary limb. Both mesenteric defects were closed with running sutures. The gastrojejunal anastomosis was hand sewn and was calibrated with a 36 Fr orogastric tube and a measurement of alimentary and biliopancreatic limbs of 100 centimeters.
As a part of diagnostic workup a fluoroscopy was performed (Figure 1) and reported an increment in the size of the blind side of the alimentary limb below the gastro-jejunal anastomosis which retained the contrast and slowed down the clearance.

An upper endoscopy was also performed (Figure 2) and reported a dilated gastro-jejunum anastomosis (around 5 cm) with a measurement of the blind end of the alimentary limb of 12 centimeters. The jejunum-jejunum anastomosis and measurement of the alimentary limb was not evaluated during the procedure.

After a thorough multidisciplinary evaluation that involved Endocrinology, Psychology, Sleep Medicine and Nutritionist specialists. The patient was offered a revisional surgery.
Intraoperative findings
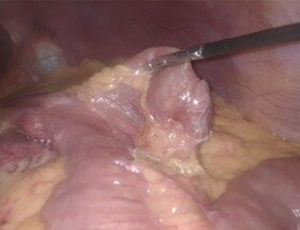
Laparoscopic evaluation revealed a long blind end of the alimentary limb below the gastro-jejunal anastomosis (Figure 3).
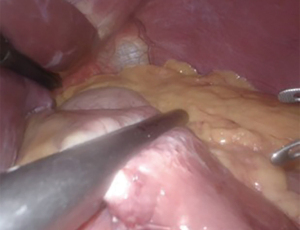
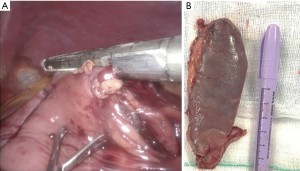
Given the preoperative endoscopy findings (enlarged gastro-jejunum anastomosis) a total remodelation of the anastomosis was performed. The gastric pouch was transected just above the previous anastomosis (Figure 4). The alimentary limb was also transected with total exclusion of the blind dilated segment (candy cane) (Figure 5A). A totally manual anastomosis was performed and calibrated with an orogastric tube (36 Fr).
The resected segment was extracted through one of the 12 mm trocars and finally measured (Figure 5B).
Both Petersen’s and intermesenteric defects were evaluated and visualized closed. Measurement of alimentary limb and biliopancreatic was also evaluated. The procedure was performed without any intraoperative complication.
The patient cursed an uneventful postoperative period. Fluoroscopic examination was performed and revealed no leaks or strictures (Figure 6). She was discharged on the second postoperative day.
During clinical follow up at six months after revisional surgery the patient experienced total remission of upper gastrointestinal symptoms. A marked improvement on weight loss was observed (27 kg). Close clinical follow up should be guaranteed.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Bariatric surgery is one of the most important alternatives for the treatment of obesity and their comorbidities. CCS is an unusual postoperative complication following LGBP. Abdominal pain, nausea and even suboptimal postoperative weight loss can be important clinical manifestations that require a thorough clinical assessment in order to rule the entity.
CCS is often underreported, only a few reports have been published in medical literature. It can present early during the postoperative period or even years after surgery. The size of blind limb could be variable.
The patient presented in this case report referred unexpected weight loss after surgery as the main complaint. She presented complete resolution of symptoms after a successful revisional surgery.
Conclusions
An adequate surgical technique can reduce the incidence of this pathology. Performing a fluoroscopy assessment early during the postoperative period can be useful leading to an early identification.
Optimal treatment for CCS implies surgical revision with remodeling or resection of the proximal dilated end of the alimentary limb. The management of CCS with endoscopy therapy has also been described as an alternative approach with satisfactory results (5,6).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-23-5/rc
Peer Review File: Available at https://ls.amegroups.com/article/view/10.21037/ls-23-5/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-23-5/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kamocka A, McGlone ER, Pérez-Pevida B, et al. Candy cane revision after Roux-en-Y gastric bypass. Surg Endosc 2020;34:2076-81. [Crossref] [PubMed]
- Kellogg TA. Revisional bariatric surgery. Surg Clin North Am 2011;91:1353-71. x. [Crossref] [PubMed]
- Robert M, Pelascini E, Poncet G, et al. Blind biliary limb dilatation (Candy cane syndrome) of jejuno-jejunal anastomosis after Roux en Y Gastric Bypass (with video). J Visc Surg 2018;155:239-41. [Crossref] [PubMed]
- Aryaie AH, Fayezizadeh M, Wen Y, et al. "Candy cane syndrome:" an underappreciated cause of abdominal pain and nausea after Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis 2017;13:1501-5. [Crossref] [PubMed]
- Rio-Tinto R, Huberland F, Van Ouytsel P, et al. Magnet and wire remodeling for the treatment of candy cane syndrome: first case series of a new approach (with video). Gastrointest Endosc 2022;95:1247-53. [Crossref] [PubMed]
- Greenberg I, Braun D, Eke C, et al. Successful treatment of "candy cane" syndrome through endoscopic gastrojejunal anastomosis revision. Clin J Gastroenterol 2021;14:1622-5. [Crossref] [PubMed]
Cite this article as: Paz-Fernandez A, León-Cabral P, Pérez-González B, Sierra-Salazar M, Martel-Vilchis A, Gallardo-Chávez V. Candy cane syndrome related with weight loss failure after laparoscopic gastric bypass: a case report. Laparosc Surg 2023;7:14.