Amyand’s hernia and ischemic omentum due to omental torsion: a case report
Highlight box
Key findings
• Laparoscopy was used to confirm diagnosis, and for treatment in a patient who presented with ischemic omentum due to torsion and Amyand’s hernia, with subsequent resolution of symptoms.
What is known and what is new?
• In cases where the diagnosis of Amyand’s hernia is unclear, laparoscopy may be used for establishing diagnosis and therapeutically.
• Treatment options for confirmed cases of ischemic omentum consist of conservative management and surgical management.
• This is the first case report describing surgical management of Amyand’s hernia and ischemic omentum due to torsion in conjunction.
What is the implication, and what should change now?
• In the case of an unclear diagnosis, or competing diagnoses, laparoscopy provides a diagnostic and therapeutic option.
Introduction
Ischemic omentum and Amyand’s hernia are both rare diagnoses seldom reported together. Only one prior case report described both findings together, and in that case the ischemic omentum was contained within the hernia sac, mimicking acute scrotum (1).
Twisting of the omentum on its pedicle with subsequent infarction of distal omentum is a described cause of abdominal pain that presents with nonspecific symptoms, and often mimics other causes of acute abdomen (2-5). Additionally, Amyand’s hernia—an inguinal hernia containing the appendix within the hernia sac—may contain an acutely inflamed appendix and present with abdominal pain (6,7).
We are presenting the case of a patient with separate findings of an Amyand’s hernia and ischemic omentum with a point of torsion, managed laparoscopically. We present the following case in accordance with the CARE reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-22-51/rc).
Case presentation
A 33-year-old male presented to the emergency department with a primary complaint of four days of lower abdominal pain that was worsening, as well as no bowel movements for the past two days. His pain was worse on the right side. He had no prior medical or surgical history. Vitals were within normal limits on arrival, and the patient denied any fever or chills, nausea or vomiting, or any urinary changes. On physical exam his abdomen was soft but he had tenderness in the bilateral lower abdominal quadrants. He also had a hernia in the right groin with tenderness, and without overlying skin changes. Labs were unremarkable, he did not have a leukocytosis or left shift. Alvarado score was 3. CT abdomen and pelvis was obtained, which showed a right inguinal hernia containing appendix and a small amount of fluid, as well as stranding of 12 cm × 12 cm fat in the right lower quadrant extending across the midline, concerning for infarcted omentum (Figure 1).
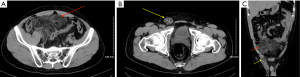
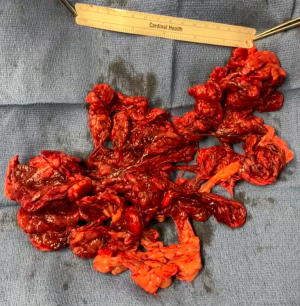
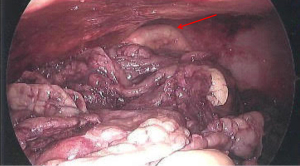
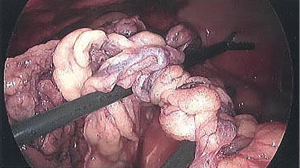
Due to the abdominal tenderness and worsening of symptoms over four days, it was unclear if the symptoms were caused by the ischemic omentum or acute appendicitis. The decision was made to take the patient to the operating room for a diagnostic laparoscopy with possible appendectomy and possible omental resection. The abdomen was entered above the umbilicus with a 10mm Hassan port. Two additional 5mm working ports were placed in the left flank, and right upper quadrant lateral to the rectus muscle. Upon entering the abdomen, serohemorrhagic fluid was identified and the pelvic omentum was ischemic. The patient was placed in Trendelenburg position with right side up. The cecum was grasped with an endoscopic Babcock and pulled towards the left upper quadrant. Using an atraumatic grasper, the ischemic omentum was dissected away until the base of the appendix was identified, with the remainder in the hernia sac. With further traction, the appendix was removed from the hernia sac. The appendix was hyperemic and nonperforated (Figure 2). An appendectomy was performed using a Harmonic to divide the mesentery and an endoscopic stapler to divide the appendix at the base of the cecum. Next the area of omental torsion was identified in the mid abdomen (Figure 3), and healthy appearing tissue proximally was divided with a harmonic. No ischemic omentum was contained within the hernia. The ischemic omentum was bluntly separated from the surrounding small bowel, abdominal wall, and pelvic structures. After dissection, the specimen was removed (Figure 4) through the supraumbilical port site. Due to inflammation, the right inguinal hernia was not fixed during the index operation. No operative drain was left.
Pathology revealed omental tissue with marked vascular congestion, focal necrosis, and inflammation. The appendix did not display evidence of acute appendicitis.
The patient was kept on IV antibiotics for 24 hours postoperatively. His pain improved and he was discharged on postoperative day 2.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Follow up
The patient had an uneventful recovery from the initial surgery and was seen in clinic two weeks postoperatively. He underwent an open right inguinal hernia repair with mesh six weeks later. He was seen two weeks after inguinal hernia repair and recovered uneventfully.
Discussion
Ischemic omentum is a rare cause of abdominal pain, and is often misdiagnosed or found during surgical intervention for other suspected pathology. Symptoms may mimic other causes of abdominal pain, most commonly acute appendicitis, making diagnosis difficult (1-5).
Omental infarction is most commonly caused by torsion, which can be primary or secondary. Primary omental torsion involves twisting on its access with vascular compromise. The etiology is unclear, but factors associated with primary torsion include anatomic malformations, variations in omental fat distribution, and anomalies of blood supply or pedicle formation. Secondary omental torsion is associated with another pathology, such as abdominal adhesion, hernia, mass, cyst, or tumor (1,8).
Treatment options for confirmed cases of ischemic omentum consist of conservative management and surgical management with laparoscopy or open surgery (2,3,9).
CT scans allow for more accurate diagnosis of ischemic omentum, and help rule out other causes of acute abdominal pain such as appendicitis, cholecystitis, diverticulitis, among others (6). If imaging is non-diagnostic, or other pathology is suspected, laparoscopy provides both diagnostic and therapeutic ability with minimal morbidity (4,9,10).
Amyand’s hernia is an uncommon inguinal hernia where the appendix is in the hernia sac (10-12). The incidence of Amyand’s hernia is approximately 1% of all hernia cases, and the incidence of acute appendicitis within the hernia is approximately 0.07–0.13% (13). In cases where the diagnosis of Amyand’s hernia is unclear multiple sources support the use of laparoscopy for establishing diagnosis and therapeutically (6).
Literature supports appendectomy in cases of an inflamed appendix, however, there is no consensus on whether to keep or remove the appendix when the appendix is normal appearing.
Losanoff and Basson (2008) developed a classification for Amyand’s hernias to represent different clinical scenarios that they encountered, which identifies four main types: Type 1, normal appendix within the hernia sac; Type 2, acute appendicitis in the hernia with inflammatory changes confined to the hernia sac; Type 3, acute appendicitis in the hernia sac with abdominal wall or peritoneal sepsis; and Type 4, acute appendicitis in the hernia sac with other abdominal pathology (7). For types 3 and 4 it is recommended to perform appendectomy and to avoid mesh (11).
The findings of Amyand’s hernia with ischemic omentum have only been described in one prior case report. The paper described the case of a five-year-old who was found to have an inguinal hernia containing a perforated appendix with infarcted omentum within the hernia sac (1).
Our patient had a different presentation and symptoms than the prior reported case. In our case the ischemic omentum was not contained in the hernia with the appendix. Preoperatively we obtained a CT scan showing both an Amyand’s hernia and evidence of infarcted omentum. Since both pathologies could explain the patient’s pain and symptom onset, we elected to manage this case laparoscopically.
Conclusions
Ischemic omentum secondary to torsion can be managed conservatively or surgically. In the case of any question about diagnosis, such as another abdominal pathology, laparoscopy should be strongly considered as both a diagnostic and therapeutic procedure. In our case a subsequent Amyand’s hernia complicated the diagnosis, and the patient was taken for laparoscopy with appendectomy and resection of ischemic omentum.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-22-51/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-22-51/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Khorramirouz R, Bagheri A, Sahebpour AA, et al. Amyand's Hernia Complicated by Omental Infarct Presenting as Acute Scrotum: Report of a Case and Review of the Literature. Case Rep Surg 2015;2015:741353. [Crossref] [PubMed]
- Park TU, Oh JH, Chang IT, et al. Omental infarction: case series and review of the literature. J Emerg Med 2012;42:149-54. [Crossref] [PubMed]
- Modaghegh MH, Jafarzadeh R. Primary omental torsion in an old woman: imaging techniques can prevent unnecessary surgical interventions. Case Rep Med 2011;2011:541324. [Crossref] [PubMed]
- Gargano T, Maffi M, Cantone N, et al. Secondary omental torsion as a rare cause of acute abdomen in a child and the advantages of laparoscopic approach. European J Pediatr Surg Rep 2013;1:35-7. [Crossref] [PubMed]
- Gupta R, Farhat W, Ammar H, et al. Idiopathic segmental infarction of the omentum mimicking acute appendicitis: A case report. Int J Surg Case Rep 2019;60:66-8. [Crossref] [PubMed]
- Morales-Cárdenas A, Ploneda-Valencia CF, Sainz-Escárrega VH, et al. Amyand hernia: Case report and review of the literature. Ann Med Surg (Lond) 2015;4:113-5. [Crossref] [PubMed]
- Losanoff JE, Basson MD. Amyand hernia: a classification to improve management. Hernia 2008;12:325-6. [Crossref] [PubMed]
- Karayiannakis AJ, Polychronidis A, Chatzigianni E, et al. Primary torsion of the greater omentum: report of a case. Surg Today 2002;32:913-5. [Crossref] [PubMed]
- Costi R, Cecchini S, Randone B, et al. Laparoscopic diagnosis and treatment of primary torsion of the greater omentum. Surg Laparosc Endosc Percutan Tech 2008;18:102-5. [Crossref] [PubMed]
- Naffaa LN, Shabb NS, Haddad MC. CT findings of omental torsion and infarction: case report and review of the literature. Clin Imaging 2003;27:116-8. [Crossref] [PubMed]
- Shaban Y, Elkbuli A, McKenney M, et al. Amyand's hernia: A case report and review of the literature. Int J Surg Case Rep 2018;47:92-6. [Crossref] [PubMed]
- Sharma H, Gupta A, Shekhawat NS, et al. Amyand's hernia: a report of 18 consecutive patients over a 15-year period. Hernia 2007;11:31-5. [Crossref] [PubMed]
- Medina-Gallardo NA, Curbelo-Peña Y, Stickar T, et al. Omental infarction: surgical or conservative treatment? A case reports and case series systematic review. Ann Med Surg (Lond) 2020;56:186-93. [Crossref] [PubMed]
Cite this article as: Krosser A, Ghirardo S. Amyand’s hernia and ischemic omentum due to omental torsion: a case report. Laparosc Surg 2023;7:11.