
Laparoscopic treatment of small bowel obstruction caused by Chilaiditi syndrome in an elderly patient: a case report
Highlight box
Key findings
• Laparoscopic surgery may be a safe and effective modality for diagnosis and treatment in patients without a surgical history and who are highly suggestive of Chilaiditi syndrome, especially in elderly patients.
What is known and what is new?
• Chilaiditi syndrome may cause small bowel obstruction in a virgin abdomen.
• Laparoscopic surgery may be a good treatment option for elderly patients diagnosed with Chilaiditi syndrome.
What is the implication, and what should change now?
• Laparoscopic surgery is feasible in patients who are highly suggestive of Chilaiditi syndrome, even in elderly patients.
Introduction
Chilaiditi syndrome is an extremely rare condition with an incidence of 0.025–0.28%. It is caused by the interposition of the bowel between the liver and right diaphragm (1). Most patients with this intestinal anomaly are asymptomatic; however, abdominal pain, constipation, vomiting, respiratory distress, anorexia, and abdominal distension are possible presentations. It may self-resolve and rarely require a surgical intervention. It is considered a rare cause of intestinal obstruction (2). The majority of reported cases requiring surgical intervention involved colonic interpositions. We present the rare case of an 85-year-old woman diagnosed with a small bowel obstruction caused by Chilaiditi syndrome, which was successfully treated with laparoscopic surgery. We present the following case in accordance with the CARE reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-22-49/rc).
Case presentation
An 85-year-old woman presented to the emergency department with obstipation. She denied having such symptoms previously. She also denied fever, chills, dyspnea, melena, and hematochezia. Her medical history included hypertension and hyperlipidemia, controlled with atorvastatin, cilostazol, amitriptyline, and losartan. The patient had no surgical history.
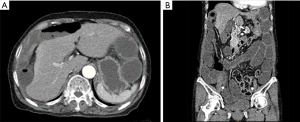
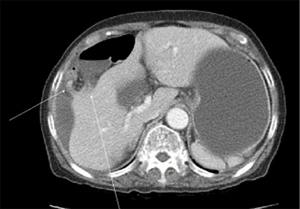
On initial presentation, she was afebrile with a blood pressure of 150/80 mmHg, pulse rate of 88 beats/min, respiratory rate of 18 beats/min, and normal oxygen saturation of 95% on room air. The cardiovascular and respiratory examinations were unremarkable. The abdomen was soft and mildly distended. She was tender on palpation in the epigastric area and right upper quadrant. Murphy’s sign was equivocal, and no signs of rebound tenderness or guarding were observed. In the initial laboratory findings, a complete blood count showed leukocytosis (16,830/µL, normal range: 4,000–10,800/µL), and white blood cell (WBC) differential count was significant for a left shift of 89% neutrophilia (normal range: 42–75%). The chemistry and coagulation panels were unremarkable. Abdominal X-ray and computed tomography (CT) revealed a dilated loop of the small bowel with hepato-diaphragmatic interposition. Additionally, a focal beak-like obstruction of the small bowel in the right upper quadrant was revealed on CT (Figure 1). As these findings suggested Chilaiditi syndrome and the patient had no surgical history, we decided to start with conservative management. The patient was managed with intravenous fluid hydration, nasogastric tube decompression, and pain management. She showed gradual improvement with conservative management up to 5 days after hospitalization. Later, despite conservative management, no further improvement was seen, and she continued to experience nausea and persistent abdominal pain without any relief. A follow-up CT scan was performed a week after she was hospitalized to determine whether a surgical intervention was required because her vital signs continued to be normal and laboratory results, including WBC, were within the normal range. When compared to the initial CT scan, the follow-up CT scan revealed a slightly aggravated state of small bowel loop dilatations in the perihepatic space (Figure 2). Based on the patient’s presentation and radiological imaging, laparoscopic exploration was performed.
One 12-mm trocar was placed above the umbilicus for camera insertion, and two 5-mm working ports were placed in the left mid-abdomen. In the laparoscopic view, two adhesive bands were observed between the dome of the liver and diaphragm. These adhesions exhibited violin-string shapes. A short segment of the small bowel became trapped between the two bands, forming a dilated loop that appeared to cause bowel obstruction. The bands were sharply lysed using an energy device (Harmonic Scalpel®, Ethicon), without any damage to the small bowel (Figure 3A-3C). The small bowel was reduced and evaluated from the ligament of Treitz to the ileocecal valve following the lysis of the adhesive bands. All bowels appeared healthy and pinkish, and no suspected ischemic change was seen. The patient had an uneventful postoperative recovery course and was discharged on the fifth postoperative day.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In 1910, the Greek radiologist Demetrius Chilaiditi described three patients with temporary hepato-diaphragmatic interposition of the colon. Therefore, a Chilaiditi sign describes the incidental radiological finding of asymptomatic hepato-diaphragmatic intestinal interposition. The term “Chilaiditi syndrome” is used for cases in which a Chilaiditi sign is accompanied by clinical symptoms (3). The most common are abdominal symptoms such as abdominal pain, nausea, vomiting, or constipation, followed less frequently by respiratory distress and angina-like chest pain (3).
A Chilaiditi sign is an extremely rare condition, and its prevalence in the general population is 0.025–0.28% (1). The sign is more prevalent in males than in females by approximately four-fold and typically involves the hepatic flexure or transverse colon, although interposition of the small bowel has also been reported (2,4). The interposition of the small bowel loop is rare, occurring in approximately 3–5% of Chilaiditi signs. Patients present with symptoms more frequently when the small bowel is interposed (5).
Initial treatment of Chilaiditi syndrome should include conservative management, including intravenous fluid hydration, bowel decompression, stool softeners, and enema. If the patient is unresponsive to conservative treatment or if there is evidence of bowel ischemia, surgical intervention should be attempted (3).
CT is the best imaging modality for the diagnosis of Chilaiditi syndrome, especially in cases of small bowel interposition (4,5). In our case, a CT scan was used to diagnose Chilaiditi syndrome with an interposed small bowel between the liver and diaphragm. Additionally, by performing follow-up CT scans, the response to conservative treatment can be evaluated and the need for surgical intervention can be determined. Our patient had persistent pain despite laboratory findings and vital signs within the normal range. Since the patient was elderly, it was necessary to be cautious in deciding on surgical intervention. Thus, we performed a follow-up CT scan to determine the need for surgical intervention. Subsequently, laparoscopic exploration was performed by analyzing the radiological evaluation and clinical presentation of the patient.
The etiology of Chilaiditi syndrome can be congenital or acquired. Normal positioning of the suspensory ligaments of the liver, mesocolon, and falciform ligament prevents intestinal interposition between the liver and diaphragm (6). Predisposing factors include reduced liver dimensions, atrophic liver, dolichocolon, and congenital abnormalities such as absent suspensory or falciform ligaments or redundant colon. Acquired risk factors include conditions that elevate the right hemidiaphragm, such as eventration or phrenic nerve injury, liver cirrhosis, obesity, chronic constipation, and surgical history (4-6).
A case report related to small bowel interposition described that a lower threshold for surgical intervention may be necessary in patients with a surgical history (6). However, in our case, the patient did not have any of the relatively well-known risk factors, including a surgical history. Violin-string adhesions between the dome of the liver and diaphragm, which are typical signs of Fitz-Hugh-Curtis syndrome (FHCS), were observed in the laparoscopic view. FHCS refer to perihepatitis associated with pelvic inflammatory disease (PID). Although two-thirds of patients with FHCS present with right abdominal pain, patients diagnosed with intestinal obstruction are rare (7,8). Until now, small bowel obstructions associated with FHCS that require surgical intervention have rarely been described. As in previous reports, our patient had no history of PID or gynecological symptoms (5,9,10). However, considering that laparoscopic observation of the typical signs of violin-string adhesions plays an important role in diagnosis (8), it was thought that our patient also developed Chilaiditi syndrome caused by FHCS.
Conclusions
In conclusion, Chilaiditi syndrome may cause small bowel obstruction in a virgin abdomen. However, it may not be considered for diagnosis because it is rare compared to other frequent causes such as gallstone ileus, inguinal hernia, internal hernia, inflammatory bowel disease, and malignancy (9). Physicians should be aware that right upper quadrant pain mimicking cholecystitis is observed in patients with Chilaiditi syndrome. CT can not only diagnose Chilaiditi syndrome but can also be used to determine the need for surgical intervention. Minimally invasive surgery can accomplish favorable postoperative outcomes in elderly patients if surgical intervention is performed at an appropriate time before bowel ischemia occurs. Laparoscopic exploration may be a safe and effective modality for diagnosis and treatment in patients without a surgical history and who are highly suggestive of Chilaiditi syndrome.
Acknowledgments
Funding: This work was supported by the Soonchunhyang University Research Fund and the National Research Foundation of Korea (NRF) grant funded by the Korean Government (No. 2021R1C1C1005884).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-22-49/rc
Peer Review File: Available at https://ls.amegroups.com/article/view/10.21037/ls-22-49/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-22-49/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Takahashi K, Ito H, Katsube T, et al. Treatment of Chilaiditi syndrome using laparoscopic surgery. Asian J Endosc Surg 2017;10:63-5. [Crossref] [PubMed]
- Mateo de Acosta Andino DA, Aberle CM, Ragauskaite L, et al. Chilaiditi syndrome complicated by a closed-loop small bowel obstruction. Gastroenterol Hepatol (N Y) 2012;8:274-6. [PubMed]
- Moaven O, Hodin RA. Chilaiditi syndrome: a rare entity with important differential diagnoses. Gastroenterol Hepatol (N Y) 2012;8:276-8. [PubMed]
- Kang D, Pan AS, Lopez MA, et al. Acute abdominal pain secondary to chilaiditi syndrome. Case Rep Surg 2013;2013:756590. [Crossref] [PubMed]
- Oh SN, Rha SE, Byun JY, et al. Chilaiditi syndrome caused by Fitz-Hugh-Curtis syndrome: multidetector CT findings. Abdom Imaging 2006;31:45-7. [Crossref] [PubMed]
- Fiumecaldo D, Buck L. Chilaiditi's Syndrome Causing High-Grade Small-Bowel Obstruction Requiring Exploratory Laparotomy. Mil Med 2018;183:e281-3. [Crossref] [PubMed]
- Faré PB, Allio I, Monotti R, et al. Fitz-Hugh-Curtis Syndrome: A Diagnosis to Consider in a Woman with Right Upper Quadrant Abdominal Pain without Gallstones. Eur J Case Rep Intern Med 2018;5:000743. [PubMed]
- Sarli L, Villa F, Iusco DR. The value of laparoscopy in the diagnosis and therapy of violin-string like perihepatic nonpostoperative adhesions. Surg Endosc 2001;15:323. [Crossref] [PubMed]
- Al-Ghassab RA, Tanveer S, Al-Lababidi NH, et al. Adhesive Small Bowel Obstruction due to Pelvic Inflammatory Disease: A Case Report. Saudi J Med Med Sci 2018;6:40-2. [Crossref] [PubMed]
- Burton E, McKeating J, Stahlfeld K. Laparoscopic management of a small bowel obstruction of unknown cause. JSLS 2008;12:299-302. [PubMed]
Cite this article as: Yun JH, Jung HI. Laparoscopic treatment of small bowel obstruction caused by Chilaiditi syndrome in an elderly patient: a case report. Laparosc Surg 2023;7:12.


