
Reduced-port robotic pancreatectomy: a narrative review of the literature
Introduction
Minimally invasive surgery (MIS) has shown an upward trend in many surgical fields worldwide. In the pancreatic field, surgical technology has undergone innovative developments in recent decades, including surgery for advanced pancreatic cancer and the introduction of MIS. While open pancreatectomies are systematized, minimally invasive pancreatectomy (MIP) is expected to reduce morbidity and is believed to have significant advantages, such as lower pain, less blood loss, and shorter time to adjuvant therapy (1). However, there remain several limitations, such as the difficulty of the MIP due to the location of the pancreas, which led to fewer laparoscopic pancreatectomies being performed, compared to other abdominal surgeries. Currently, laparoscopic distal pancreatectomy (LDP) is accepted globally, as it is comparable to open surgery in terms of feasibility and safety (1,2). However, general gastroenterological surgeons who commonly perform open pancreaticoduodenectomy (PD) may not be able to perform laparoscopic PD (LPD), because of the complex procedures involved, namely, dissection around the superior mesenteric vein, portal vein, and superior mesenteric artery, and reconstruction with laparoscopic limitations (3-5). Apart from LDP, LPD is still performed by a limited number of expert surgeons worldwide. Robotic surgery involves surgical innovations such as motion scaling, tremor reduction, and an internal articulated wrist (6). In addition to these features, the inclusion of three-dimensional visualization and up to seven degrees of freedom facilitates the performance of robotic distal pancreatectomy (RDP) and robotic PD (RPD).
MIS allows for other perspectives that should be considered in the development of reduced-port surgery (RPS). This technique, which is often called the “single-port” or “single-site” surgery, without depending on the number of lesions, is expected to be less invasive than conventional laparoscopic surgery (7,8). RPS has organically become common worldwide. However, it is associated with technical limitations, including instrumental collisions owing to difficulties in triangulation; numerous procedural improvements and new technologies are necessary to accomplish RPS laparoscopically. However, robotic systems can overcome this issue as they enable flexible articulation of instruments. Although many studies on RPS have been published in various surgical robotics fields (9-11), there are fewer reports of robotic RPS in pancreatic field than those of robotics in other fields because of the complexity and difficulty.
Although reduced-port robotic pancreatectomy (RPRP) is still not widely recognized, several expert surgeons have attempted to perform RPRP in recent years. Most of these attempts are for RDP, but reduced-port RPD (RPRPD) is being performed at a small number of institutions, including ours. Herein, we present the current status and evaluate the feasibility of RPRP in terms of future prospects. We present the following article in accordance with the Narrative Review reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-22-47/rc).
Review strategy
We searched for original manuscripts on RPRP, published before May 30, 2022, in the PubMed, Embase, and Cochrane databases. The following terms were used to perform the search: (I) “robotic” or “robot-assisted”; (II) “pancreatectomy”, “pancreatic surgery”, “pancreaticoduodenectomy”, “pancreatoduodenectomy”, or “Whipple”; and (III) “reduced-port”, “single-port”, “single-site”, or “single-incision”. The list of potentially matched studies was analyzed. As few reports were expected, the data of studies written in English were analyzed without setting a lower limit on the number of cases or without excluding the pathological outcomes, including case reports. Complications were standardized according to the Clavien-Dindo classification (12), and a postoperative pancreatic fistula (POPF) was defined as a pancreas-specific complication according to the guidelines of the International Study Group on Pancreatic Surgery (13). Two authors independently screened the papers for. Because this was a narrative review, ethical approval was not required. The search strategy was summarized in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | June 10, 2022 |
| Databases and other sources searched | PubMed, Embase, Cochrane databases |
| Search terms used | (I) “robotic” or “robot-assisted” |
| (II) “pancreatectomy”, “pancreatic surgery”, “pancreaticoduodenectomy”, “pancreatoduodenectomy”, or “Whipple” | |
| (III) “reduced-port”, “single-port”, “single-site”, or “single-incision” | |
| Timeframe | 2010–May 30, 2022 |
| Inclusion and exclusion criteria | Any type of articles written in English, including a case report |
| Selection process | The articles were screened by the first author |
RPRP
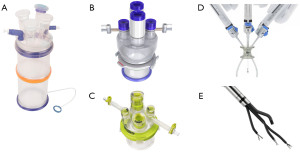
Few reports on RPRP exist; we were able to find only seven studies, including one case report (Tables 2,3). In total, 104 RPRP cases were reported in the literature, including 59 cases of reduced-port RDP (RPRDP) and 45 cases of RPRPD. RPRP was first performed by Kim et al., who reported a single-site plus one-port RDP in 2017 (14). Patient background and reduced-port technique details are presented in Table 2. Although the participants in these studies varied in age range, generally, RPRPs were not performed in severely obese patients. Figure 1 shows the single-port platforms used in the RPRP in this review. During the console time, various commercial single-port platforms were adopted to perform RPRP, such as the Glove port® (Nellis, Bucheon, Korea), LAGIPORT® (LAGIS, Taichung), Uni Port® (Dalim Medical, Seoul, Korea), and Da Vinci single-site platform (DVSSPTM, Intuitive Surgical, Sunnyvale, CA, USA), using a small incision through or around the umbilicus. The Da Vinci SP system (Intuitive Surgical, Sunnyvale, CA, USA) was used by two institutions for single-site surgery, including in one case report (20). Interestingly, Choi et al. used these platforms for both single-port and additional ports (18).
Table 2
| Author | Year | N | Procedure | Age (years) | BMI (kg/m2) | Patient selection | Single-port platform | Number of additional port |
|---|---|---|---|---|---|---|---|---|
| Kim et al. (14) | 2017 | 5 | DP | 38 [21–56]† | N/A | Benign and low grade malignancy | DVSSPTM | Plus one |
| Peng et al. (15) | 2018 | 10 | DP | 50.4 [36–67]‡ | N/A | Benign and malignancy | LAGIPORT® | Pure single-port |
| Han et al. (16) | 2019 | 13 | DP | 46.1±14.0§ | 20.9±4.0† | Benign and low grade malignancy | DVSSPTM | Plus one |
| Park et al. (17) | 2020 | 27 | DP | 47.3 [21–74]‡ | 22.6 [15.8–28.8]‡ | Benign and low grade malignancy | Glove port® | Plus one |
| Choi et al. (18) | 2022 | 3 | DP | 70.7 [65–77]‡ | 27.8 [24.9–30.7]‡ | Benign and early staged pancreatic cancer | Uni port® and Da Vinci SP system | Plus one |
| Chiang et al. (19) | 2022 | 45 | PD | 66 [61–73]† | 23# | Malignant tumor | Glove port® | Pure single-port or plus one |
| Liu et al. (20) | 2022 | 1 | DP | 55 | N/A | Serous cystadenoma | Da Vinci SP system | Plus one |
†, median [range]; ‡, mean [range]; §, mean ± standard deviation; #, mean. BMI, body mass index; DP, distal pancreatectomy; N/A, not available; DVSSP, Da Vinci single-site platform; PD, pancreaticoduodenectomy.
Table 3
| Author | Year | N | Procedure | Spleen preservation* | Operation time (min) |
Estimated blood loss (mL) | Complication more than II* | POPF grade > B* | Postoperative hospital stay (days) | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| Kim et al. (14) | 2017 | 5 | DP | 1 (20.0) | 165 [120–270]† | 5 [0–50]† | N/A | 0 | 6 [5–8]† | 1; converted to multi-port |
| Peng et al. (15) | 2018 | 10 | DP | 2 (20.0) | 252.5 [210–295]‡ | 149.0 [50–250]‡ | 3 (30.0) | 0 | 4.5 [3–6]‡ | – |
| Han et al. (16) | 2019 | 13 | DP | 1 (7.7) | 192±69§ | 12±22§ | 5 (38.5) | 0 | 7.4±1.9§ | – |
| Park et al. (17) | 2020 | 27 | DP | 9 (33.3) | 201 [118–488]‡ | 50 [0–700]‡ | 1 (3.7) | 0 | 7 [4–10]‡ | 1; converted to multi-port |
| Choi et al. (18) | 2022 | 3 | DP | 0 (0.0) | 215 [135–265]‡ | <500 | 0 (0.0) | 0 | 11 [10–11]‡ | – |
| Chiang et al. (19) | 2022 | 45 | PD | N/A | 325 [290–370]† | 300 [155–700]† | 7 (15.6) | 1 (2.2) | 32 [25–50]† | 3; converted to open |
| Liu et al. (20) | 2022 | 1 | DP | 1 (100.0) | 55 | 20 | 0 | 0 | 3 | – |
Complications were presented as per the Clavien-Dindo classification. *, values are presented as n (%); †, median [range]; ‡, mean [range]; §, mean ± standard deviation. POPF, postoperative pancreatic fistula; DP, distal pancreatectomy; N/A, not available; PD, pancreaticoduodenectomy.
Regarding RPRDP, there were five reports on the single-site plus one-port technique (14,16-18,20), and only one report on single-port RDP in the narrow sense, that is, a pure single-site surgery, which was performed by Peng et al. (15). Han et al. evaluated and compared the perioperative outcomes of single-site plus one-port RDP and pure single-site LDP (16). Only Park et al. demonstrated a similar technique with multicenter (six centers) outcomes (17). Median patient age less than 60 years in five of seven studies can be attributed to the fact that many patients with benign diseases were included in the studies.
Spleen preservation was performed in 14 (23.7%) patients. Although the spleen preserving distal pancreatectomy (DP) procedure is supposed to be more complicated than the conventional DP procedure, Yang et al. described that the spleen preservation rate was significantly higher in the RPRDP group than in the single-site LDP group (21). Although the details are unknown, the spleen preservation rate of 23.7% in these reports does not lead to preclusion of RPRDP for such cases. Two cases were converted to multi-port RDP (3.4%) because of the difficulty caused by collision and obesity, respectively. The perioperative outcomes are presented in Table 3. RPRDP is a safe procedure in terms of operative time, blood loss, serious complications, and hospital stay, and the development of RPRDP is expected to continue.
All RPRPDs were described in only one report (19). Chiang et al. compared 45 cases of RPRPD with 13 cases of open PD for malignant tumors and found that the amount of blood loss was lower in the RPRPD group than in the open PD group {300 [95% confidence interval (CI): 155–700] vs. 650 mL (95% CI: 300–850), P=0.11} but RPRPD group had the longer operative time correspond to open PD group [325 (95% CI: 290–370) vs. 215 min (95% CI: 180–270), P<0.001]. The data for the RPRPD study were collected by a single surgeon who performed pure single-site RDP in Taiwan, and included only patients with malignant tumors of the pancreas or periampullary regions; patients who underwent RPRPD for benign tumors were excluded. Interestingly, Peng et al. (15), who also performed pure single-site surgery in RDP, did not require an additional port in 13 of 45 cases (28.9%) of RPRPD. Three patients (6.7%) required conversion to open surgery. Although there is only one previously published report, RPRPD poses no problems regarding operative time, blood loss, or any outcomes, and it is possible that it is not associated with technical issues. Further data accumulation in this regard are expected.
Evolution of MIP
The history of pancreatic resection begins with Whipple’s successful PD in 1935 (22). In the 1940s, although surgical procedures were standardized, the associated complications and mortality rates were extremely high. In 1973, Fortner et al. proposed a concept that involved resection of the internal organs in the left upper abdomen along with total pancreatectomy, and en bloc resection along with the main vessels such as the portal vein, superior mesenteric artery, and celiac axis, as regional pancreatectomy (23).
Laparoscopic pancreatectomy was first reported by Gagner et al., in the form of LPD, in 1994 (24); Cuschieri et al. first performed LDP, in 1996 (25). Subsequently, laparoscopic pancreatic tumor enucleation and laparoscopic central pancreatectomy have also been reported (26). At that time, laparoscopic surgical devices were inadequate and less recommended. However, the use of laparoscopic surgery has since become widespread. Since the late 2000s, several studies have reported good surgical outcomes for LPD, and the operation time and outcomes have greatly improved (27-29). Currently, even though MIP has been accepted worldwide. MIS in PD remains technically challenging. One meta-analysis reported a higher mortality associated with LPD than with open PD (4).
Concurrent to the initiation of laparoscopic surgery in the late 1980s, the American military undertook development of surgical-assist robots to allow surgeons to operate on the wounded remotely, from the safety of the mainland or on-board ships away from the battlefield. In 2001, a team of surgeons at a New York hospital performed remote-controlled robotic cholecystectomy in a female patient in France (30). Since then, there have been many reports from various fields on the usefulness and expanded indications of robotic surgery, which continues to evolve. Melvin et al. reported the first case of RDP after pancreatic surgery (31). Consequently, some reports comparing LDP and RDP have reported that RDP is superior to LDP in terms of operative time, blood loss, and open conversion rate, whereas others have found them to be equivalent (32-36). Following the first report of RPD by Giulianotti et al. in 2003, numerous reviews have reported the safety and usefulness of this surgery, as it helps overcome the technical difficulties of laparoscopic pancreatectomy and is beneficial in terms of histopathological outcomes (6,37-41). It is undisputed that robotic surgery is superior to laparoscopic surgery in terms of maneuverability in the pancreatic field, and it has the potential to reduce surgical stress as a sustainable procedure with an ergonomic position.
The first successful case of reduced-port robotic surgery for humans in the urological field was reported by Kaouk et al. in 2009 as a single-site surgery (42), followed by several reports in other fields, such as gynecological and colorectal surgery, during the same period (43,44). For some time thereafter, although RPS was used in many areas, RPRP was not readily reported. To the best of our knowledge, the first RPRP was reported by Kim et al. in 2017, a decade later than that in other fields (14). Notably, even though few papers have justified it, RPS is rapidly becoming more popular worldwide as first as RPS in other fields.
Outlook
Although the small number of material papers in this review may not conclusively guide the next steps in RPRP, we initially anticipated that it would have a longer operative times than conventional robotic pancreatectomy, and that more patients would require additional ports. Nevertheless, none of the reports showed that RPRP had an inferior performance compared to that of conventional robotic pancreatectomies; however, no comparative studies have been conducted. Chang et al. reported an additional port requirement rate of 8.55% in single-site laparoscopic cholecystectomy (45); however, only five patients in this review required conversion to multi-port technique or open surgery (4.8%). This difference may indicate the feasibility of robotic surgery in pancreatic field.
Various single-port platforms have been used in RPS to reduce the complexity of the procedure. In robotic surgery, single-port platforms are classified into those traditionally used in laparoscopic surgery, and those with a platform made specifically for robotic use. The Da Vinci single-site technology with DVSSPTM has curve-designed cannulas to maximize range of motion and minimize collisions (Figure 1D). The Da Vinci SP system delivers three multi-joint instruments and a wristed camera through a single trocar (Figure 1E). There are unique to Da Vinci Surgical Systems, although some sealing devices are not available and should be used with caution in pancreatectomies with high bleeding risks. The other single-port devices presented in this review have been conventionally used in laparoscopic surgery (Figure 1A-1C). While all robotic instruments can be used in these platforms, the distance between robotic arms tends to be shorter, which facilitates instrumental collision.
The most crucial outcome factor in pancreatectomy is the POPF. The drainage tube allows for essential POPF control, which contributes to the limited feasibility of single-site surgery. Indeed, patients who underwent pure single-site surgery in this review required a new incision for drain placement. As it is possible that one tube will not be sufficient for PD, the RPRPD must be planned accordingly. Additional incisions used to introduce trocars should be used for drain placement; this will lead to the wound form being the same in pure single-site and single-site plus one-port or plus two-port surgeries. At our institution, we consider that two drainage tubes are required for PD; hence, we have been implementing RPRPD using the single-site plus two-port technique. In addition to the single-port on the umbilicus, trocars are placed on the left and right sides of the abdomen, and the robotic arms are set there. In this technique, the final wound is a similar to that formed after single-incision surgery, and instances of instrument collision can be reduced (unpublished). The requirement of additional ports may be determined based on the drainage policies of each institution. As Chiang et al. (19) also mentioned, to make the surgical field easier to handle with additional ports, the single-port plus one-port or two-port techniques should be considered for new RPRPD procedures.
While several studies have shown the feasibility of RPRP, there are some issues that prevent RPRP from being widely adopted. First, the disadvantage of RPS is its cost, which is an additional patient fees of several hundred US dollars for a single-port platform. Second, RPS is generally perceived to complicate the procedure, such as the difficulty of triangulation and the tendency of the instruments collisions. Therefore, RPS may be considered unsuitable for RPRP, which is highly difficult procedure. Therefore, further studies on a larger scale and comparative studies with conventional robotic pancreatectomies are warranted to clearly demonstrate the non-inferiority of RPRP.
Conclusions
Only 5 years have passed since RPRP was first reported, and this procedure is still in the developmental period. We hope that many more studies will be reported, including randomized control trials, in the future, and that RPRP will be commonly used worldwide.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Ippei Matsumoto) for the series “Laparoscopic Pancreatic Surgery” published in Laparoscopic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-22-47/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-22-47/coif). The series “Laparoscopic Pancreatic Surgery” was commissioned by the editorial office without any funding or sponsorship. CMP is an unpaid Director of Taiwan Robotic Surgery Association, unpaid Vice President of Taiwan Association for Endoscopic Surgery and unpaid Supervisor of Taiwan Surgical Society of Gastroenterology. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Iacobone M, Citton M, Nitti D. Laparoscopic distal pancreatectomy: up-to-date and literature review. World J Gastroenterol 2012;18:5329-37. [Crossref] [PubMed]
- Nigri GR, Rosman AS, Petrucciani N, et al. Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc 2011;25:1642-51. [Crossref] [PubMed]
- Dulucq JL, Wintringer P, Mahajna A. Laparoscopic pancreaticoduodenectomy for benign and malignant diseases. Surg Endosc 2006;20:1045-50. [Crossref] [PubMed]
- Kendrick ML, van Hilst J, Boggi U, et al. Minimally invasive pancreatoduodenectomy. HPB (Oxford) 2017;19:215-24. [Crossref] [PubMed]
- Wang M, Meng L, Cai Y, et al. Learning Curve for Laparoscopic Pancreaticoduodenectomy: a CUSUM Analysis. J Gastrointest Surg 2016;20:924-35. [Crossref] [PubMed]
- Lefor AK. Robotic and laparoscopic surgery of the pancreas: an historical review. BMC Biomed Eng 2019;1:2. [Crossref] [PubMed]
- Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, et al. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 2010;24:1842-8. [Crossref] [PubMed]
- Ayloo SM, Buchs NC, Addeo P, et al. Traditional versus single-site placement of adjustable gastric banding: a comparative study and cost analysis. Obes Surg 2011;21:815-9. [Crossref] [PubMed]
- Bae SU, Jegon WK, Baek SK. Single plus one-port robotic surgery using the da Vinci Single-Site Platform versus conventional multi-port laparoscopic surgery for left-sided colon cancer. Wideochir Inne Tech Maloinwazyjne 2022;17:179-87. [Crossref] [PubMed]
- Seo WJ, Son T, Shin H, et al. Reduced-port totally robotic distal subtotal gastrectomy for gastric cancer: 100 consecutive cases in comparison with conventional robotic and laparoscopic distal subtotal gastrectomy. Sci Rep 2020;10:16015. [Crossref] [PubMed]
- Cruz CJ, Yang HY, Kang I, et al. Technical feasibility of da Vinci SP single-port robotic cholecystectomy: a case report. Ann Surg Treat Res 2019;97:217-21. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 2017;161:584-91. [Crossref] [PubMed]
- Kim SH, Kang CM, Lee WJ. Robotic single-site plus ONE port distal pancreatectomy. Surg Endosc 2017;31:4258-9. [Crossref] [PubMed]
- Peng CM, Liu HC, Hsieh CL, et al. Application of a commercial single-port device for robotic single-incision distal pancreatectomy: initial experience. Surg Today 2018;48:680-6. [Crossref] [PubMed]
- Han HJ, Kang CM. Reduced port minimally invasive distal pancreatectomy: single-port laparoscopic versus robotic single-site plus one-port distal pancreatectomy. Surg Endosc 2019;33:1091-9. [Crossref] [PubMed]
- Park G, Choi SH, Lee JH, et al. Safety and Feasibility of Robotic Reduced-Port Distal Pancreatectomy: a Multicenter Experience of a Novel Technique. J Gastrointest Surg 2020;24:2015-20. [Crossref] [PubMed]
- Choi YJ, Jo HS, Kim DS, et al. Single-port robot plus one port (SP + 1) distal pancreatectomy using the new da Vinci SP system. Langenbecks Arch Surg 2022;407:1271-6. [Crossref] [PubMed]
- Chiang CH, Chiang CH, Cheng TC, et al. Reduced-port robotic pancreaticoduodenectomy versus open pancreaticoduodenectomy: a single-surgeon experience. Surg Today 2022;52:896-903. [Crossref] [PubMed]
- Liu R, Zhao GD, Zhang XP, et al. The first case report of single-port robot-assisted pancreatectomy using the da Vinci SP system. Intelligent Surgery 2022;1:32-5.
- Yang SJ, Hwang HK, Kang CM, et al. Revisiting the potential advantage of robotic surgical system in spleen-preserving distal pancreatectomy over conventional laparoscopic approach. Ann Transl Med 2020;8:188. [Crossref] [PubMed]
- Whipple AO, Parsons WB, Mullins CR. Treatment of carcinoma of the ampulla of vater. Ann Surg 1935;102:763-79. [Crossref] [PubMed]
- Fortner JG. Regional resection of cancer of the pancreas: a new surgical approach. Surgery 1973;73:307-20.
- Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 1994;8:408-10. [Crossref] [PubMed]
- Cuschieri A, Jakimowicz JJ, van Spreeuwel J. Laparoscopic distal 70% pancreatectomy and splenectomy for chronic pancreatitis. Ann Surg 1996;223:280-5. [Crossref] [PubMed]
- Gagner M, Pomp A, Herrera MF. Early experience with laparoscopic resections of islet cell tumors. Surgery 1996;120:1051-4. [Crossref] [PubMed]
- Palanivelu C, Jani K, Senthilnathan P, et al. Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg 2007;205:222-30. [Crossref] [PubMed]
- Kendrick ML, Cusati D. Total laparoscopic pancreaticoduodenectomy: feasibility and outcome in an early experience. Arch Surg 2010;145:19-23. [Crossref] [PubMed]
- Kim SC, Song KB, Jung YS, et al. Short-term clinical outcomes for 100 consecutive cases of laparoscopic pylorus-preserving pancreatoduodenectomy: improvement with surgical experience. Surg Endosc 2013;27:95-103. [Crossref] [PubMed]
- Marescaux J, Leroy J, Gagner M, et al. Transatlantic robot-assisted telesurgery. Nature 2001;413:379-80. [Crossref] [PubMed]
- Melvin WS, Needleman BJ, Krause KR, et al. Computer-enhanced robotic telesurgery. Initial experience in foregut surgery. Surg Endosc 2002;16:1790-2. [Crossref] [PubMed]
- Guerrini GP, Lauretta A, Belluco C, et al. Robotic versus laparoscopic distal pancreatectomy: an up-to-date meta-analysis. BMC Surg 2017;17:105. [Crossref] [PubMed]
- Benizri EI, Germain A, Ayav A, et al. Short-term perioperative outcomes after robot-assisted and laparoscopic distal pancreatectomy. J Robot Surg 2014;8:125-32. [Crossref] [PubMed]
- Butturini G, Damoli I, Crepaz L, et al. A prospective non-randomised single-center study comparing laparoscopic and robotic distal pancreatectomy. Surg Endosc 2015;29:3163-70. [Crossref] [PubMed]
- Daouadi M, Zureikat AH, Zenati MS, et al. Robot-assisted minimally invasive distal pancreatectomy is superior to the laparoscopic technique. Ann Surg 2013;257:128-32. [Crossref] [PubMed]
- Lee SY, Allen PJ, Sadot E, et al. Distal pancreatectomy: a single institution's experience in open, laparoscopic, and robotic approaches. J Am Coll Surg 2015;220:18-27. [Crossref] [PubMed]
- Giulianotti PC, Coratti A, Angelini M, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg 2003;138:777-84. [Crossref] [PubMed]
- Cirocchi R, Partelli S, Trastulli S, et al. A systematic review on robotic pancreaticoduodenectomy. Surg Oncol 2013;22:238-46. [Crossref] [PubMed]
- Müller-Debus CF, Thomaschewski M, Zimmermann M, et al. Robot-Assisted Pancreatic Surgery: A Structured Approach to Standardization of a Program and of the Operation. Visc Med 2020;36:104-12. [Crossref] [PubMed]
- Da Dong X, Felsenreich DM, Gogna S, et al. Robotic pancreaticoduodenectomy provides better histopathological outcomes as compared to its open counterpart: a meta-analysis. Sci Rep 2021;11:3774. [Crossref] [PubMed]
- Boggi U, Napoli N, Costa F, et al. Robotic-Assisted Pancreatic Resections. World J Surg 2016;40:2497-506. [Crossref] [PubMed]
- Kaouk JH, Goel RK, Haber GP, et al. Robotic single-port transumbilical surgery in humans: initial report. BJU Int 2009;103:366-9. [Crossref] [PubMed]
- Escobar PF, Fader AN, Paraiso MF, et al. Robotic-assisted laparoendoscopic single-site surgery in gynecology: initial report and technique. J Minim Invasive Gynecol 2009;16:589-91. [Crossref] [PubMed]
- Ostrowitz MB, Eschete D, Zemon H, et al. Robotic-assisted single-incision right colectomy: early experience. Int J Med Robot 2009;5:465-70. [Crossref] [PubMed]
- Chang SK, Lee KY. Therapeutic advances: single incision laparoscopic hepatopancreatobiliary surgery. World J Gastroenterol 2014;20:14329-37. [Crossref] [PubMed]
Cite this article as: Ninomiya R, Abe S, Kogure R, Beck Y, Peng CM. Reduced-port robotic pancreatectomy: a narrative review of the literature. Laparosc Surg 2023;7:4.


