Laparoscopic approaches to adrenalectomy for large adrenal tumours: a systematic review
Introduction
Laparoscopic adrenalectomy (LA) was first introduced by Gagner et al. (1) in 1992. The procedure was first described in a patient with Cushing’s syndrome due to an adrenocortical adenoma. Since then, the entire spectrum of adrenal pathology, both secretory and non secretory including non-functioning adenomas, pheochromocytomas, Cushing’s disease, Conns’ aldosteronomas, myelolipoma, and cysts are routinely treated with LA (2,3). Several studies have clearly documented and established its superiority over conventional open adrenalectomy in terms of postoperative recovery, hospital stay and overall costs and patient satisfaction. However laparoscopic surgical management of large adrenal masses is not routinely undertaken due to concerns of oncological compromise in malignancy, technical complexity of the procedure and the greater potential for intraoperative or postoperative complications.
Current contraindications for LA are adrenocortical carcinomas (ACC) with radiographic evidence of tumour invasion, recurrence of tumour after prior adrenalectomy and severe cardiopulmonary disease (4). There is also potential risk of injury to adjacent structures including kidney, liver, spleen, pancreas, inferior vena cava and bowel. Size, location and pathology of the tumour as well as surgical proficiency are factors which makes LA technically challenging. There are two primary issues to consider when approaching a large adrenal tumour laparoscopically. The first encompasses the technical challenges of removing a large adrenal tumour, which include longer surgical hours, higher blood loss, and perioperative complications. The second factor is the malignant potential of the tumour, which is proportional to the tumor size (5). The risk for partial resection, tumour spillage, and capsular disruption, which can result in local tumor recurrence and metastasis, are the main concerns with laparoscopic surgery for adrenal cancer (6).
Another factor that has driven endocrine teams to continue to recommend open surgical approach for adrenal cortical carcinoma or for large possibly malignant adrenal lesions is the risk of local or port-site recurrence (7). However urinary and serum biomarkers are increasingly contributing to definitive diagnoses of adrenocortical cancers. Because of this relative diagnostic insensitivity, size criteria continue to be used as an indicator of malignant potential, with tumors larger than 5 cm being regarded to be at high risk for malignancy (8). As a result, open surgery for large adrenal tumors is still advocated in the literature.
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) do not support laparoscopic resection for tumours believed to be malignant, especially when they are larger than 6 cm in diameter (9). For adrenal tumours smaller than 6 cm with no local invasion, the European Society of Endocrinology (ESE) recommends laparoscopic surgery. Every adrenal tumour larger than 6 cm, requires a specific surgical strategy according to the ESE (10).
While there is limited consensus on laparoscopic surgery for large adrenal tumours, there is more consensus on laparoscopic hepatectomy for hepatocellular cancers, and also for tumours in unfavourable segments (11,12). Minimally invasive approaches are also being used in very large renal masses with good outcomes (13). It would hence be logical to consider LA for large adrenal tumours also.
For a safe adrenal operation, proper preoperative planning is essential. Appropriate surgical approach for large adrenal lesions will need to be individualized to the appropriate patient and pathology. In the last 15 years, various studies have shown that the laparoscopic approach is the gold standard for adrenal lesions smaller than 5 cms (14). The size of the adrenal tumour on preoperative imaging should not be the key criterion for deciding whether or not to perform a laparoscopic procedure. This article aims to review and consolidate the evidence accumulated in the last two decades on the laparoscopic approach for large adrenal tumours. We present the following article in accordance with the PRISMA reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-22-15/rc)
Methods
A systematic review of the literature was performed by searching the PubMed database on December 20th 2021, for all relevant articles published in English between January 2010 and December 2021 on LA for large adrenal tumours. The keywords used were laparoscopy, large adrenal masses, large adrenal tumors, adrenalectomy.
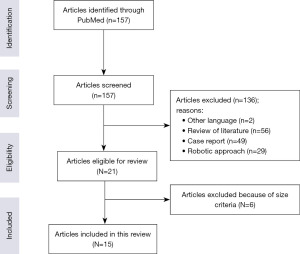
A PubMed search yielded 157 studies (Figure 1). All studies that reported outcomes of LA for large tumours (usually defined as a maximum dimension of more than 5–6 cm) as their main focus were reviewed. Letters and review articles were excluded. Duplicate data in multiple publications by the same authors were excluded as well. Additionally, Case reports and articles which focused on surgical technique or evaluating predictive factors were excluded.
Both retrospective and prospective studies were included. Newcastle-Ottawa scale was used to assess the quality of the studies. The studies included had a significant risk of bias according to Newcastle-Ottawa scale. The various laparoscopic approaches included were transperitoneal laparoscopic adrenalectomy (TPLA), retroperitoneoscopic laparoscopic adrenalectomy (RPLA), hand assisted laparoscopic adrenalectomy (HALA) and robotic adrenalectomy (RA). For the purposes of this review, only outcomes of patients undergoing transperitoneal, retroperitoneoscopic or hand assisted laparoscopic approaches were considered. Studies comparing RA with laparoscopic approach are beyond the scope of this review article and hence excluded.
Two reviewers (BV and ZM) independently screened all citations by title and abstract, followed by full-text review to reach a final decision on inclusion. The outcomes of the studies were analysed for details including numbers of patients involved, median size of the lesion, need for conversion to open, blood loss, operating time, perioperative complications and recurrence in malignancy. A database was created by both reviewers collectively on Microsoft ExcelTM with care taken to avoid duplication of data. A thorough assessment of selective non-reporting or under-reporting of results in the studies was carried out.
Results
Out of the 15 articles reviewed, 12 were retrospective studies and 3 were prospective studies. There was a global distribution of origin of the studies. The study and patient characteristics of the 15 articles is shown in Table 1.
Table 1
| Study | Year | N | Group (G): number of patients (n) | Study method | Age (years), mean ± SD/median [range] | Length of hospital stay (days), mean ± SD/median [range] |
|---|---|---|---|---|---|---|
| Değer et al. (15), Turkey | 2019 | 62 | G1 <5 cm: 46 | R | G1: 46.1±12.7 | G1: 37.6±20.9 min |
| G2 ≥5 cm: 16 | G2: 47±12.5 | G2: 49.8±22.9 min | ||||
| Zografos et al. (16), Greece | 2010 | 166 | G1<8 cm TPLA: 135 | R | All patients were between 16 to 80 years old | G1,G2: mean of 1.5 days |
| G2 ≥8 cm TPLA: 14 | G3: 5 to 20 days | |||||
| G3 ≥8 cm OA: 17 | ||||||
| Chen et al. (17), China | 2018 | 175 | G1 TPLA ≥5 cm: 37 | R | G1: 47.92±29.61 | G1: 8.91±3.40 |
| G2 RPLA ≥5 cm: 41 | G2: 44.41±38.90 | G2: 7.43±2.82 | ||||
| G3 RPLA <5 cm: 97 | G3: Not mentioned | G3: 2.07±0.36 | ||||
| Natkaniec et al. (18), Poland | 2016 | 530 | G1 TPLA <6 cm: 441 | P | G1: 55.52±13.25 | Not mentioned |
| G2 TPLA ≥6 cm: 89 | G2: 52.9±16 | |||||
| Prakobpon et al. (19), Thailand | 2021 | 456 | G1 TPLA <6 cm: 408 | R | G1: 47.4 [38–56] | G1: 4 [4–5] |
| G2 TPLA ≥6 cm: 48 | G2: 51.4 [43–60] | G2: 5.5 [5–7] | ||||
| Sahbaz et al. (20), Turkey | 2020 | 128 | G1 TPLA <6 cm: 64 | R | G1: 53 [27–76] | G1: 3 [1–9] |
| G2 TPLA ≥6 cm: 22 | G2: 47 [19–79] | G2: 3 [1–14] | ||||
| Zhao et al. (21), China | 2021 | 78 | G1: OA ≥8 cm: 38 | R | G1: 50 [38–59] | G1: 10 [8–13] |
| G2: TPLA ≥8 cm: 40 | G2: 50 [37–57] | G2: 6 [4–7] | ||||
| Agrusa et al. (22), Italy | 2014 | 41 | G1 TPLA <6 cm: 27 | P | G1: – | G1: – |
| G2 TPLA ≥6 cm: 14 | G2: 55.6 [38–74] | G2: 4.2 [3–6] | ||||
| Cicek et al. (23), Turkey | 2021 | 330 | G1 TPLA <6: 277 | P | G1: 50.9±12.5 | G1: 3±1.6 |
| G2 TPLA ≥6: 53 | G2: 49.7±12.7 | G2: 3.7±3.5 | ||||
| Bozkurt et al. (24), Turkey | 2015 | 35 | G1 TPLA ≥8 cm: 16 | R | G1: 55.2±8.6 | G1: 2+0.8 |
| G2 TPLA <8 cm: 19 | G2: 50.1±11.4 | G2: 2.3+0.6 | ||||
| Dalvi et al. (25), India | 2012 | 46 | TPLA ≥5 cm: 46 | R | 33.6 [16–62] | 4 [2–8] |
| Carter et al. (26), USA | 2012 | 26 | G1 TPLA <6 cm: 15 | P | G1: 51±3 | G1: 1±0 |
| G2 TPLA ≥6 cm: 11 | G2: 57±4 | G2: 2±1 | ||||
| Hwang et al. (27), Korea | 2014 | 133 | G1 RPLA <5 cm: 57 | R | G1: 50.86±14.17 | G1: 7.88±3.08 |
| G2 RPLA ≥5 cm: 76 | G2: 50.95±14.03 | G2: 9.26±3.10 | ||||
| Buxton et al. (28), UK | 2019 | 56 | HALA ≥5 cm (56 patients) | R | 52 [17–82] | 6 [2–21] |
| Zhu et al. (29), China | 2019 | 147 | G1: RPLA (n=101) | R | G1: 47.15±12.9 | G1: 7 [4–12] |
| G2: OA (n=46) | G2: 45.17±10.29 | G2: 9 [5–14] | ||||
| Pheochromocytomas ≥5 cm |
R, retrospective; P, prospective; TPLA, transperitoneal laparoscopic adrenalectomy; RPLA, retroperitoneal laparscopic adrenalectomy; OA, open adrenalectomy.
Nine out of 15 of the studies compared outcomes of TPLA in patients with large and small adrenal masses. Two of the studies compared TPLA with OA in patients with large adrenal masses. One study compared outcomes of TPLA approach with RPLA, while compared outcomes of RPLA with OA. One study each dealt with RPLA and HALA individually. Six out of 14 cohort studies had ≥5 cm as the size criteria for large adrenal tumours. Two out of the six, compared outcomes of TPLA in lesions <5 cm and ≥5 cm.
No significant difference between these groups in terms of operative time and blood loss were noticed by Değer et al. (15) comparing 16 lesions ≥5 cm and 46 lesions <5 cm. Similarly, Dalvi et al. (25) concluded that LA is safe and feasible for large adrenal lesions. However in that series there were 5 conversions out of 46 patients to open surgery and 1 mortality due to metastasis three months after surgery. Most of the patients in this study had pheochromocytoma and the mean size was 7.03 cm with range of 5 to 15 cm.
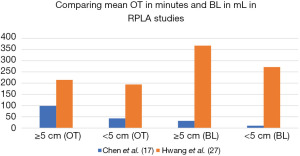
Chen et al. (17) compared transperitoneal laparoscopic approach in adrenal tumours ≥5 cm with the retroperitoneal approach in such lesions and concluded that RPLA was superior to TPLA in terms of operation time, hospitalisation duration, time to first oral intake and time to ambulation. The mean tumour size overall was 5.78±1.29 cm in this study. In comparing RPLA in the ≥5 cm tumour and <5 cm tumour groups, the frequency of conversions to open surgery, number of perioperative complications, time to first oral intake and the time to ambulation did not differ significantly. The ≥5 cm group, on the other hand, had a prolonged operation time, higher blood loss, longer hospital stay and the drain was insitu for a longer time.
In a similar study with RPLA as the surgical approach, Hwang et al. (27) described adrenal lesions ≥5 cm with a mean tumour size of 7.10±2.15 cm undergoing RPLA versus lesions <5 cm undergoing RPLA. Lesions ≥5 cm had considerably higher estimated blood loss, postoperative hospitalization stay and delay in ambulation. However, the operation time and haemoglobin level change was not statistically different between groups. Difference in findings of operation time and intraoperative blood loss in these two studies comparing outcomes of RPLA in <5 cm and ≥5 cm tumours is shown in Figure 2.
In a cohort of 147 patients, Zhu et al. (29) compared the outcomes of RPLA (n=101) and OA (n=46) in pheochromocytomas larger than 5 cm. When compared to patients who had OA, the RPLA group had a shorter operational time, a faster recovery of bowel function, and a shorter post-operative stay.
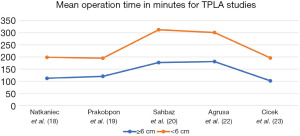
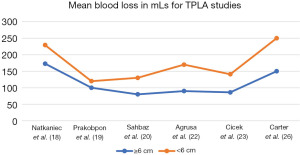
Six out of 15 cohort studies describe large adrenal tumour as ≥6 cm. This included 237 patients with adrenal lesions ≥6 cm. These studies compared TPLA in lesions <6 cm versus ≥6 cm. The open conversion was described in 3 of the studies with 16 patients undergoing open conversion out of 159 with ≥6 cm lesions. The most common reasons for conversion were bleeding or injury to adjacent structures. Post-operative and intraoperative complications were significantly higher in 2 out of 6 of the studies. Prakobpon et al. (19) compared 408 patients with tumours <6 cm and 48 patients with tumour ≥6 cm. The study described operative times, estimated blood loss, transfusion rate, intra-operative and post-operative complications which were significantly higher in the ≥6 cm group. The common intraoperative complications were tumour capsular tears, massive haemorrhage, liver injury, splenic injuries which required laparoscopic splenectomy in one patient, diaphragmatic injury and inferior vena cava injury. The 30-day postoperative complications included a patient with 9.5 cm pheochromocytoma who had hemiparesis following a ischemic stroke and patients with pleural effusions which were needle aspirated. This study also had significantly different pre-operative diagnoses between the groups.
A total of 136 patients with ≥6 cm lesions in the other 4 studies undergoing TPLA did not show significant intra-operative and post-operative complications compared to lesions <6 cm.
These 4 studies also showed no significant estimated blood loss, recurrence, or length of stay between the 2 groups.
Three studies compared outcome of transperitoneal laparoscopic approach in adrenal tumours ≥8 cm. A total of 69 patients in these three studies with ≥8 cm adrenal lesions with both benign and malignant histopathology underwent TPLA. Two of the studies compared TPLA & OA in ≥8 cm adrenal lesions and one compared TPLA in ≥8 cm vs. <8 cm adrenal lesion. The mean operative time and blood loss were comparable. Out of the 69 patients, 2 had to be converted to open surgery in view of difficult dissection. In all the 3 studies, the post-operative complications were comparable to open surgery in similar sized adrenal tumours and laparoscopic approach to <8 cm lesions.
Buxton et al. (28) looked at outcomes of HALA in tumours ≥5 cm and concluded that HALA was a safe and repeatable adrenal surgery approach that combined laparoscopic surgery with tactile integration. Open conversion was lower compared to other reported TPLA studies. The postoperative complication rates were self-limiting and higher than the rate for TPLA but lower than OA.
Tumour recurrence was reported by Zografos et al. (16), where a patient with 10 cm × 6.5 cm potentially malignant adenoma had recurrence at 5 years after LA. This required open resection of the recurrent tumour along with partial nephrectomy. There was no recurrence noted in the other 14 cohort studies.
Overall survival (OS) of patients was mentioned in two of the studies. Zhao et al. (21) report a Median OS of OA group with tumour size ≥8 cm as 70 (40–120) months and TPLA group with tumour size ≥8 cm as 15 (10–38) months. Agrusa et al. (22) reports 2 patients in TPLA group with tumour size ≥6 cm, had malignant tumors. Both patients with malignant pheochromocytoma and incidental adrenal cortical cancer were still alive respectively after 15 and 36 months of follow-up. Other studies did not have significant ACC to evaluate OS.
Table 2 depicts the outcome characteristics of the evaluated studies and Table 3 provides an overview of the studies evaluated in this article.
Table 2
| Study | Operative time (min), mean ± SD/median [range] | Mean blood loss (mL), mean ± SD/median [range] | surgical complications | Conversion to open surgery | Recurrence/follow up (month), mean ± SD/median [range] |
Overall survival |
|---|---|---|---|---|---|---|
| Değer et al. (15), Turkey | G1: 101.2±21.8 | G1: 49.5 | G1: 2 | G2: 1 | No recurrence/2.3±1.8 years | Not mentioned |
| G2: 107.4±25.4 | G2: 94.3 | G2: 1 | ||||
| Zografos et al. (16), Greece | G1: 65 to 240 | G1, G2: minimal | G1: 2 | G1: 1 | 1 patient from G2/8 years | Not mentioned |
| G2: 150 to 240 | ||||||
| Chen et al. (17), China | G1: 124.36±34.62 | G1: 136.34±19.83 | G1: 1 | Not mentioned | Not mentioned | Due to lack of sufficient malignant tumors, survival analysis not done |
| G2: 98.71±32.30 | G2: 31.93±20.0 | G2: 0 | ||||
| G3: 42.63±18.51 | G3: 10.29±6.04 | G3: 1 | ||||
| Natkaniec et al. (18), Poland | G1: 86.6±35 | G1: 56.5±114.4 | G1: 41 | G1: 2 | Not mentioned | Not mentioned |
| G2: 111.9±43.7 | G2: 172.8±220.6 | G2: 14 | G2: 6 | |||
| Prakobpon et al. (19), Thailand | G1: 75 [60–108] | G1: 20 [20–50] | G1: 22 | G1: 1 | Not calculated due to low ACC cases | – |
| G2: 120 [100–150] | G2: 100 [30–300] | G2: 15 | G2: 7 | |||
| Sahbaz et al. (20), Turkey | G1: 135.5 ±66.3 | G1: 50 [10–300] | G1: 1 | G1: 3 | Not calculated due to low ACC cases | Not mentioned |
| G2: 177.1 ±69.9 | G2: 80 [25–150] | G2: 1 | G2: 3 | |||
| Zhao et al. (21), China | G1: 215 [180–240] | G1: 1000 [625–1500] | G1: 10 | Not mentioned | G1: 65 [38–118] | G1: 70 [40–120] |
| G2: 180 [135–245] | G2: 200 [100–700] | G2: 11 | G2: 14 [9–36] | G2: 15 [10–38] | ||
| Agrusa et al. (22), Italy | G1: mean 120 min | G1: mean 80 mL | G1: – | G1: 0 | G2-two had malignant tumors. Both patients with malignant pheochromocytoma and incidental adrenal cortical cancer were still alive respectively after 15 and 36 months of follow-up | – |
| G2: 181 [145–240] | G2: mean 90 mL | G2: 1 | G2: 0 | |||
| Cicek et al. (23), Turkey | G1: 94.4±35.8 | G1: 55±44.2 | G1: 2 | G1: 1 | Not mentioned | – |
| G2: 101.6±39.9 | G2: 86.2 ±70.4 | G2: 5 | G2: 0 | |||
| Bozkurt et al. (24), Turkey | G1: 113.4±41.0 | G1: 141.9±80.5 | G1: 12 | G1: 1 | No recurrence/mean 22 months follow-up | Not mentioned |
| G2: 103.2±20.2 | G2: 100.5±40.1 | G2: 8 | G2: 1 | |||
| Dalvi et al. (25), India | 144 [45 – 270] | 112 [20 – 400] | Not mentioned | 5 | Not mentioned | – |
| Carter et al. (26), USA | Not mentioned | G1: 100 [50–150] | G1: 1 | G1: 0 | No recurrence | Not mentioned |
| G2: 150 [50–1200] | G2: 2 | G2: 0 | G1: 50±8 | |||
| G2: 55±11 | ||||||
| Hwang et al. (27), Korea | G1: 194.12±69.34 | G1: 271.75±232.98 | G1: 11 | G1: 0 | No follow up | – |
| G2: 214.54±76.04 | G2: 367.24±275.11 | G2: 13 | G2: 0 | |||
| Buxton et al. (28), UK | 144 [69–287] | Not mentioned | 8 | 1 | Not mentioned | – |
| Zhu et al. (29), China | G1: 185 [89–520] | G1: 150 [50–2300] | G1: 39 | G1: 6 | G1: 42.6 [2.8–118.8] | Not applicable |
| G2: 245 [107–480] | G2: 500 [50–3000] | G2: 16 | G2: 70.8 [4.0–117.5] |
Table 3
| Study | Outcomes | Conclusion | Newcastle-Ottawa scale (Selection score + comparability score + outcome score)-Max score 9 |
|---|---|---|---|
| Değer et al. (15), Turkey | No statistically significant difference between groups in terms of operative time and blood loss. Length of hospital stay longer in G2. One conversion to open in G2 due to ruptured capsule. Postoperative complications were similar | LA can be applied safely in experienced centres in masses ≥5 cm with no suspected invasion on preoperative imaging | 4+2+3=9 |
| Zografos et al. (16), Greece | Mortality and major morbidity did not differ in patients with large tumours when compared with patients with smaller tumours. One patient in G2 had recurrence of potential malignancy after 5 years and underwent open curative resection | Laparoscopic resection of large (≥8 cm) adenal tumors is feasible and safe. Short- and long-term results did not differ in the 3 groups | 4+2+3=9 |
| Chen et al. (17), China | RPLA was superior to TPLA in terms of operation time, hospitalization duration, time to first oral intake and time to ambulation. G2 showed superior results for the intraoperative indicators than the G3, while the results for the postoperative indicators were similar | Both RPLA and TPLA provide similar effects for the surgical management of large adrenal tumours | 4+0+3=7 |
| Natkaniec et al. (18), Poland | Duration of surgery & intraoperative blood loss was significantly higher in G2. There was a linear relationship between tumour size and the duration of surgery, and between tumour size and intraoperative blood loss. Postoperative complications and conversion to open were comparable | TPLA of tumours ≥6 cm is more difficult, but it can be regarded safe and beneficial for patients | 4+2+1=7 |
| Prakobpon et al. (19), Thailand | Patients in G2 had higher median operative time, estimated blood loss, transfusion rate, conversion rate, intra/post-operative complications and length of postoperative stays than in G1 | TPLA in large adrenal tumour ≥6 cm is feasible but associated with significantly worse intraoperative complications, postoperative morbidity, and recovery. However, most of the complications were minor and could be managed conservatively. Careful patient selection with surgical expertise in adrenal surgery is the key factor for successful laparoscopic surgery in large adrenal tumours | 4+2+3=9 |
| Sahbaz et al. (20), Turkey | The conversion rate was similar between the two groups. The duration of surgery, morbidity and lengths of hospital stay were similar | LA can be safely performed on adrenal masses over 6 cm | 4+1+3=8 |
| Zhao et al. (21), China | The median operation time was comparable. The median blood loss was higher in OA compared to LA group On univariate and multivariate analysis, the larger diameter of tumour was significantly associated with operation time, blood loss, and recovery time | LA was found to be safe and feasible in experienced hands and can replace open surgeries in most cases. Radiology and endocrinologic profile characterizing the tumour play a predominant role in the determination of the optimal surgical approach | 4+2+3=9 |
| Agrusa et al. (22), Italy | Mean blood loss was comparable. No conversion to open surgery was required | LA is safe and feasible for adrenal masses larger than 6 cm. In the presence of local invasion or vascular infiltration laparoscopic approach is contraindicated | 4+0+0=4 |
| Cicek et al. (23), Turkey | Postoperative complications and blood loss were more significant in G2. Length of hospital stay was comparable | 6 cm should not be considered as an upper limit of TPLA in lesions without suspicion of adrenal primary malignancy and may be safely performed in centres with experience | 4+1+1=7 |
| Bozkurt et al. (24), Turkey | Operation time and blood loss were comparable. Conversion to an open procedure required in two patients, one from each group, because of the firm adherence of adrenal mass to the surrounding tissue | LA is a safe and feasible procedure for large lesions even up to 15 cm. The risk of finding incidental adrenal cortical cancer was significantly increased for large lesions in this series as in the literature; therefore, it is important to follow the strict oncological principles in these cases | 4+2+3=9 |
| Dalvi et al. (25), India | The average blood loss was 112 mL with the mean operating time being 144 min. Five patients required conversion to open adrenalectomy. 3 patients (6.52%) on final histology had malignant tumours | LA is safe and feasible for large adrenal lesions. Mere size should not be considered as a contraindication to laparoscopic approach in large adrenal masses. A graded approach, good preoperative assessment, team work and adherence to anatomical, surgical and oncological principles are the key to successful outcomes | Not applicable |
| Carter et al. (26), USA | There was no significant difference in intra-operative complications, estimated blood loss, cancer diagnosis, or recurrence. The length of stay was comparative between the two cohorts and there were no incidents of capsular invasion or adverse cardiovascular events | Laparoscopic adrenalectomy of pheochromocytomas larger than 6 cm is feasible and safe with comparable results to smaller lesions | 4+1+3=8 |
| Hwang et al. (27), Korea | The estimated blood loss, time to ambulation and postoperative hospitalization were significantly higher in G2 but operative time and drop in haemoglobin were comparable. No patients experienced conversion to open surgery | RPLA can be used in patients with tumours larger than 5 cm | 4+2+1=7 |
| Buxton et al. (28), UK | • Post operative complications in 14% (all self limiting) | Hand assisted laparoscopic surgery offers a safe reproducible approach to adrenal surgery combining minimally invasive surgery with tactile integration. HALA is a safe minimally invasive surgical option for larger tumours, including malignancies. The HALA technique may additionally offer a shorter learning curve for trainee adrenal surgeons | Not Applicable |
| • 1 (1.8%) open conversion | |||
| • 1 (1.8%) recurrence with successful clearance on repeat surgery | |||
| • Median length of stay was 6 days | |||
| Mihai et al. (30), UK | Adrenal tumours with extension into major venous structures should all be approached through an open operation. Large phaeochromocytomas of up to 8–10 cm might still be approached laparoscopically by surgeons with appropriate experience but the larger the diameter of such tumours the more likely is that open adrenalectomy will be necessary. Bilateral adrenalectomy is not an indication for open approach as laparoscopic or retroperitoneoscopic surgery is feasible in these patients | Patients with large adrenocortical tumours (>6–8 cm) and those with CT suspicion of locally invasive tumours expected to have an adrenocortical cancer should have an open operation. In addition, laparoscopic adrenalectomy should be converted to open operation in case there is macroscopic appearance suspicious of malignancy (invasion in surrounding structures, presence of regional lymphadenopathy) or if the surgeon is concerned that the tumour could not be removed without avoiding tumour fragmentation/spillage | Not Applicable |
| Zhu et al. (29) | RPLA patients have shorter operative time, quicker return of bowel function and shorter length of hospital stay when compared to the OA group | RPLA is safe and effective in large pheochromyctomas (≥5 cm in size) | 4+2+3=9 |
LA, laparscopic adrenalectomy; TPLA, transperitoneal laparoscopic adrenalectomy; RPLA, retroperitoneal laparscopic adrenalectomy; OA, open adrenalectomy; HALA, hand assisted laparoscopic approach.
Discussion
Minimally invasive surgery is fully established in almost all surgical specialities as it has been shown to have significant and obvious patient benefits and satisfaction. Advances in minimally invasive techniques have been helped along with advances in technology and laparoscopic instrumentation. An example of such advances is laparoscopic liver resections for large lesions and also for HCC, which is being undertaken.
LA is considered the gold standard approach for smaller secreting or non-secreting adrenal lesions, including bilateral lesions. Several studies that have compared laparoscopic approach with open surgery have shown that minimally invasive procedures are associated with lower hospital stay, post-operative disability, and complication rates.
There is however debate around laparoscopic approaches to larger adrenal lesions. The controversies around the laparoscopic approach, to large adrenal lesions are primarily due to the increased incidence of malignancy in larger adrenal tumours, with the potential of tumour spillage, incomplete oncological clearance, and recurrence.
Technical skills in laparoscopic surgery for large adrenal tumours also are of crucial importance, due to the low incidence of such tumours and the relative sparse experience of operators, except in high volume referral centres. It is evident from published studies that the best surgical approach depends on size of the lesion, body habitus of the patient, and the surgeon’s expertise. The most important measures are a technically uncomplicated procedure with full resolution of pathology, and in the case of adrenal malignancies a full oncological clearance. There is universal consensus that adrenal lesions encroaching into major venous structures should undergo open adrenalectomy.
Large phaeochromocytomas up to 10 cm in diameter may still be treated with LA by experienced surgeons, but the bigger the tumor diameter, the more likely it is that conversion to open adrenalectomy will be required (29). However, most of the studies evaluated in this review support a laparoscopic approach with better post operative outcomes provided there is the required surgical expertise.
Minimally invasive adrenalectomy can be divided into transperitoneal (TPLA), retroperitoneal (RPLA), hand assisted laparoscopic approach (HALA) and RA. The transperitoneal approach, is aided by larger working space with instrumental manouverability, more visibility, as well anatomical familiarity. However, TPLA requires retraction of abdominal organs, introducing a higher risk for injury to surrounding structures. A prolonged ileus, as well as the possibility of adhesion development and pulmonary complications, are all potential side effects of TPLA (17). In patients who have had previous abdominal surgery, TPLA may be technically challenging. From the studies reviewed, comparing outcomes in TPLA in large adrenal tumours the most common reason for conversion was bleeding or injury to adjacent structure. Post-operative and intraoperative complications were significant in only 2 out of the 6 studies with our studies showing no significant difference in the post-operative and intraoperative complication including organ injury or vascular injury. These 4 studies also showed no significant blood loss, recurrence, or length of stay. The mean operating time between groups is shown in Figure 3 and mean blood loss in Figure 4. The discrepancy in the distribution of mean operating time and blood loss between studies show that experience of the surgeon plays a major role in the outcome of TPLA for large lesions.
RPLA has inherent advantages; it has a more direct approach to the adrenals and therefore avoids intra-abdominal organs and structures. However, the restricted potential laparoscopic working space limits the extent of the removable portion of the tumour. The limited pneumoperitoneum leads to modify technique due to limited movement of instruments. Many studies have reported that while RPLA can be used for small to medium-sized benign adrenal lesions its utility for larger lesions is limited. The 2 studies reviewed in this study comparing RPLA in tumours ≥5 cm with tumors <5 cm showed higher intra-operative estimated blood loss, longer operation time and duration of hospital stay seen in the group with large adrenal lesion undergoing RPLA compared to the smaller lesions. However RPLA was found to be safe and effective with better short term outcomes for patients with large pheochromocytomas when compared with OA (29) and associated with similar outcomes with shorter operative time when compared to TPLA (17). The discrepancy in the outcomes again point towards the fact that surgical experience and skill plays a major role in the outcomes of laparoscopic approach
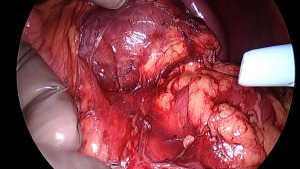
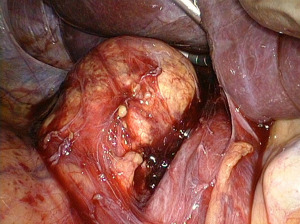
In HALA the advantages of the procedure are laparoscopic approach combined with the tactile advantage of the surgeon’s hands in assisting with retraction and dissection of the tissue planes (Figure 5), the ability to exert compression for haemostasis in the scenario of a bleed (Figure 6) and dissection speed. It allows for the treatment of larger lesions that would be difficult to treat with a solely laparoscopic technique, especially in the case of malignant disease processes. However, lesions larger than 6 cm will require a bigger incision for extraction, losing the advantage of the pure endoscopic approach. HALA therefore provides a good balance when compared to the totally endoscopic approach (28) (Figure 7).

The main point of note in the laparoscopic approach to larger tumours is the concerns regarding total oncologic clearance of primary malignant adrenal lesions. Case reports of local recurrence and peritoneal dissemination following laparoscopic procedures for primary malignancies back up these concerns (31-33). Recurrence might occur as a result of inadequate excision or capsular disruption during manipulation of the adrenal mass. The review identified only one recurrence where the patient underwent open resection including partial nephrectomy after 5 years of primary surgery. Several studies have clearly established that long-term survival rates using laparoscopic methods are comparable to those with open surgery and have significant improvement in postoperative quality of life.
We aimed to complete this review under the PRISMA guidance but several limitations remain. This study’s main limitation is the articles selected and available in the literature are all non-randomized retrospective analyses making it subject to publication and selection bias along with underpowering due to the limited data available comparing various techniques in surgery for large adrenal tumours. Failure to perform subgroup analysis based on confounding factors along with heterogeneity in evaluation indices are other limitations. This review is therefore not designed to prove the superiority of one technique over the other, but to demonstrate the feasibility of the various laparoscopic approaches in the management of large adrenal tumours. Thus, a prospective randomized trial is ideally needed to investigate which technique may be the best.
In conclusion, a review of current literature affirms the safety and efficacy of LA as long as the operator is skilled and experienced, and strictly follows oncological principles after robust evaluation and diagnosis. Patients with locally advanced tumours or vascular invasions that may necessitate en-bloc excision of nearby organs are not candidates for LA. LA can be considered for large (≥6 cm) and potentially malignant adrenal tumours. If local invasion is suspected intraoperatively, the procedure should be promptly switched to OA. Both TPLA and RPLA are safe and effective techniques for large tumours although RPLA may provide shorter operative times and reduced risk of postoperative ileus. The ideal laparoscopic approach, however, should be determined not just by tumour size but by the experience and expertise of the surgical team. The laparoscopic hand assisted technique is an especially useful but underutilized method for tumours at the upper end of the size spectrum.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Robert Sutcliffe) for the series “Laparoscopic Adrenalectomy” published in Laparoscopic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-22-15/rc
Peer Review File: Available at https://ls.amegroups.com/article/view/10.21037/ls-22-15/prf
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-22-15/coif). The series “Laparoscopic Adrenalectomy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gagner M, Lacroix A, Bolté E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. N Engl J Med 1992;327:1033. [Crossref] [PubMed]
- Suzuki K, Kageyama S, Hirano Y, et al. Comparison of 3 surgical approaches to laparoscopic adrenalectomy: a nonrandomized, background matched analysis. J Urol 2001;166:437-43. [Crossref] [PubMed]
- Lezoche E, Guerrieri M, Feliciotti F, et al. Anterior, lateral, and posterior retroperitoneal approaches in endoscopic adrenalectomy. Surg Endosc 2002;16:96-9. [Crossref] [PubMed]
- Murphy MM, Witkowski ER, Ng SC, et al. Trends in adrenalectomy: a recent national review. Surg Endosc 2010;24:2518-26. [Crossref] [PubMed]
- Li L, Yang G, Zhao L, et al. Baseline Demographic and Clinical Characteristics of Patients with Adrenal Incidentaloma from a Single Center in China: A Survey. Int J Endocrinol 2017;2017:3093290. [Crossref] [PubMed]
- Wu K, Liu Z, Liang J, et al. Laparoscopic versus open adrenalectomy for localized (stage 1/2) adrenocortical carcinoma: Experience at a single, high-volumecenter. Surgery 2018;164:1325-29. [Crossref] [PubMed]
- Lee MJ, Hahn PF, Papanicolaou N, et al. Benign and malignant adrenal masses: CT distinction with attenuation coefficients, size, and observer analysis. Radiology 1991;179:415-8. [Crossref] [PubMed]
- Hobart MG, Gill IS, Schweizer D, et al. Laparoscopic adrenalectomy for large-volume (> or = 5 cm) adrenal masses. J Endourol 2000;14:149-54. [Crossref] [PubMed]
- Stefanidis D, Goldfarb M, Kercher KW, et al. SAGES guidelines for minimally invasive treatment of adrenal pathology. Surg Endosc 2013;27:3960-80. [Crossref] [PubMed]
- Fassnacht M, Arlt W, Bancos I, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 2016;175:G1-G34. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Usai S, Del Basso C, Levi Sandri GB. Anatomically unfavorable segments: laparoscopic and robotic liver resection in posterosuperior segments and the caudate lobe, a narrative review. Laparosc Surg 2022;6:3. [Crossref]
- Grimaud LW, Chen FV, Chang J, et al. Comparison of Perioperative Outcomes for Radical Nephrectomy Based on Surgical Approach for Masses Greater Than 10 cm. J Endourol 2021;35:1785-92. [Crossref] [PubMed]
- Rosoff JS, Raman JD, Del Pizzo JJ. Laparoscopic adrenalectomy for large adrenal masses. Curr Urol Rep 2008;9:73-9. [Crossref] [PubMed]
- Değer M, İzol V, Akdoğan N, et al. Is Laparoscopic Adrenalectomy Safe in Large Adrenal Masses? Bull Urooncol 2019;18:7-11.
- Zografos GN, Farfaras A, Vasiliadis G, et al. Laparoscopic resection of large adrenal tumors. JSLS 2010;14:364-8. [Crossref] [PubMed]
- Chen W, Liang Y, Lin W, et al. Surgical management of large adrenal tumors: impact of different laparoscopic approaches and resection methods on perioperative and long-term outcomes. BMC Urol 2018;18:31. [Crossref] [PubMed]
- Natkaniec M, Pędziwiatr M, Wierdak M, et al. Laparoscopic Transperitoneal Lateral Adrenalectomy for Large Adrenal Tumors. Urol Int 2016;97:165-72. [Crossref] [PubMed]
- Prakobpon T, Santi-Ngamkun A, Usawachintachit M, et al. Laparoscopic transperitoneal adrenalectomy in the large adrenal tumor from single center experience. BMC Surg 2021;21:68. [Crossref] [PubMed]
- Sahbaz NA, Dural AC, Akarsu C, et al. Transperitoneal laparoscopic surgery in large adrenal masses. Wideochir Inne Tech Maloinwazyjne 2020;15:106-11. [Crossref] [PubMed]
- Zhao J, Ma W, Xie J, et al. Laparoscopic Treatment of Large Adrenal Tumor is Safe and Effective? A Single Center Experiences. J Invest Surg 2021;34:957-62. [Crossref] [PubMed]
- Agrusa A, Romano G, Frazzetta G, et al. Laparoscopic adrenalectomy for large adrenal masses: single team experience. Int J Surg 2014;12:S72-4. [Crossref] [PubMed]
- Cicek MC, Gunseren KO, Senol K, et al. Is 6 cm Diameter an Upper Limit for Adrenal Tumors to Perform Laparoscopic Adrenalectomy? J Laparoendosc Adv Surg Tech A 2021;31:301-5. [Crossref] [PubMed]
- Bozkurt IH, Arslan M, Yonguc T, et al. Laparoscopic adrenalectomy for large adrenal masses: Is it really more complicated? Kaohsiung J Med Sci 2015;31:644-8. [Crossref] [PubMed]
- Dalvi AN, Thapar PM, Thapar VB, et al. Laparoscopic adrenalectomy for large tumours: Single team experience. J Minim Access Surg 2012;8:125-8. [Crossref] [PubMed]
- Carter YM, Mazeh H, Sippel RS, et al. Safety and feasibility of laparoscopic resection for large (≥ 6 CM) pheochromocytomas without suspected malignancy. Endocr Pract 2012;18:720-6. [Crossref] [PubMed]
- Hwang I, Jung SI, Yu SH, et al. Is larger tumor size a contraindication to retroperitoneal laparoscopic adrenalectomy? World J Urol 2014;32:723-8. [Crossref] [PubMed]
- Buxton J, Vun SH, van Dellen D, et al. Laparoscopic hand-assisted adrenalectomy for tumours larger than 5 cm. Clin Endocrinol (Oxf) 2019;90:74-8. [PubMed]
- Zhu W, Wang S, Du G, et al. Comparison of retroperitoneal laparoscopic versus open adrenalectomy for large pheochromocytoma: a single-center retrospective study. World J Surg Oncol 2019;17:111. [Crossref] [PubMed]
- Mihai R. Open adrenalectomy. Gland Surg 2019;8:S28-35. [Crossref] [PubMed]
- Chen B, Zhou M, Cappelli MC, et al. Port site, retroperitoneal and intra-abdominal recurrence after laparoscopic acrenalectomy for apparently isolated metastasis. J Urol 2002;168:2528-9. [Crossref] [PubMed]
- Foxius A, Ramboux A, Lefebvre Y, et al. Hazards of laparoscopic adrenalectomy for Conn's adenoma. When enthusiasm turns to tragedy. Surg Endosc 1999;13:715-7. [Crossref] [PubMed]
- Hamoir E, Meurisse M, Defechereux T. Is laparoscopic resection of a malignant corticoadrenaloma feasible? Case report of early, diffuse and massive peritoneal recurrence after attempted laparoscopic resection. Ann Chir 1998;52:364-8. [PubMed]
Cite this article as: Varghese B, Moinuddin Z, Augustine T. Laparoscopic approaches to adrenalectomy for large adrenal tumours: a systematic review. Laparosc Surg 2022;6:38.