
Advantages of minimally invasive approach for inguinal bladder hernia repair: case report and literature review
Introduction
Inguinal bladder hernia (IBH) is a rare disease, accounting for 0.5% of all inguinal hernias (1). Given to the rarity of the disease, patients with IBH are at risk for misdiagnosis during preoperative evaluation. Indeed, acute kidney injury (AKI), or even multiorgan failure (MOF) might be a result of delayed diagnosis (2,3). Upon diagnosis being made, open hernioplasty has been the treatment of choice; however, literature reviews have demonstrated that some patients with IBH have been treated with ipsilateral open hernioplasty (4,5). There are some advantages of a laparoscopic approach in such cases, specifically to the laparoscopic extended-totally extraperitoneal (eTEP) to be discussed. We present the following case in accordance with the CARE reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-21-19/rc).
Case presentation
We report on two cases of IBH and the literature review, using the following method: we conducted the literature search on Ovid (Medline), using the MeSH term: inguinal hernia, bladder hernia or “inguinal bladder hernia”, herniorrhaphy, and hernioplasty. The results were limited to an adult population, in the English language and between 2011 and 2021; last search date was on August 4, 2021.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (approval No. REC.64-406-10-3) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Clinical case 1
The first case was a 60-year-old, male presenting with a right groin mass for 1 year, without urinary symptoms. He was diagnosed with indirect inguinal hernia (IIH) and underwent an open hernioplasty. During the operation, we found 4 cm × 3 cm sized, sac-like structures with complete separation from the spermatic cord, protruding medially to the inferior epigastric vessels; suspected for urinary bladder. To confirm that the sac-like structures were from the urinary bladder, saline insufflation via a Foley’s catheter was used (Figure 1). Once confirmation was made, the urinary bladder was reduced, unopened to the extraperitoneal space. Light-weighted, polypropylene mesh, 15 cm × 10 cm in size, was used and completion of hernioplasty via the Lichtenstein technique was performed. The postoperative period was uneventful, the patient was discharged on postoperative day 2 and there was no clinical evidence of recurrence on follow-up at 6 months.

Clinical case 2
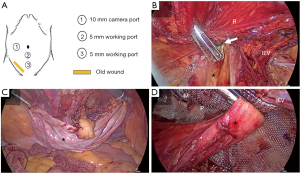
For the second case, a 67-year-old, male presented with a right groin mass, with difficult urination for 1 year. He was diagnosed as having a direct inguinal hernia with benign prostatic hypertrophy (BPH), and underwent open hernioplasty via the Lichtenstein technique. On postoperative day 4, he had a recurrent, irreducible tendered right scrotal mass, 5 cm × 5 cm in size, that extended from the most medial part of the inguinal area (Figure 2); this was accompanied with marked abdominal distension. His preoperative diagnosis was recurrent hernia with small bowel obstruction (SBO). Our decision was to undertake a posterior approach, using the eTEP technique (Video S1). The eTEP was selected instead of TEP because of two reasons: first, a short distance between an umbilicus and pubic tubercle, second, an incarceration of hernia which might causing a narrow view in TEP. Under general anesthesia, the patient was placed in the supine position. Ports placement are shown in Figure 3A. The retro-rectus space was created using a Hegar’s dilator and balloon spacer. We performed dissection of the retropubic as well as the lateral space, until reaching the anterior-superior iliac of the spine. Identification of spermatic contents confirmed no IIH component. The hernia defect (Figure 3B) was located through the anterosuperior to the pubic tubercle area, corresponding to the superficial inguinal ring externally (Figure 2). The content was reduced back; thus, clearly confirming the urinary bladder (Figure 3C), and was then reduced to its anatomical position. The pseudosac (transversalis fascia) was then fixed with the abdominal wall. Three-dimension mesh, 10 cm × 15 cm in size, was placed over the defect and the myopectineal orifices (Figure 3D).

The postoperative period was uneventful, the patient was discharged on postoperative day 5. The patient was free of urinary symptoms, and there was no clinical evidence of recurrence on follow-up at 7 months.
Literature review
Thirty-four original articles, with 73 cases of IBH have been reported over the past decade; 75 cases including this present report, with most IBHs being diagnosed preoperatively (2-4,6-27); accounting for 93.3% (70 of 75 patients). Computed tomography (CT) scanning is the imaging of choice in 26 of 34 articles (2-4,6,7,9-11). Of the total, 4.0% (3 of 75 patients) were diagnosed during operation (5,23). Surprisingly, 10.7% (8 of 75 patients) had surgical repair of their ipsilateral inguinal hernias (4-6,22,23), with only two patient undergoing transabdominal preperitoneal (TAPP) repair (15,22). The most common three presentations were: urinary frequency (14-16,18,21,22,24,27-29), two-stage urination (3,8,12,15,19,23,24,26,28,30,31) and AKI (2,3,9-11,21,27,32-34) accounting for 17.3%, 16.0% and 12.0%, respectively. It was also noticed that one-third of the patient are asymptomatic and five patients presenting with only an inguinal mass without urinary symptoms (5,20). Summary of reported cases are presented in Table 1. The possible presenting symptoms and signs are summarized in Table 2.
Table 1
| Authors | n | Clinical presentations† | Previous hernia repair | Time of diagnosis | Diagnostic test | Surgical approach | Complications | Recurrence‡ (month) |
|---|---|---|---|---|---|---|---|---|
| Bernhardson et al. (4), 2021 | 1 | Urinary retention | Ipsilateral, open | Pre-op | CT scan | Open | Bladder injury | No (N/A) |
| Tome et al. (6), 2021 | 1 | Scrotal pain, hematuria, oliguria | Bilateral, robotic | Pre-op | CT scan | Open | N/A | N/A |
| Levi et al. (2), 2020 | 1 | Urinary retention, hematuria, AKI | No | Pre-op | CT scan | Open | ESRD | No (N/A) |
| Gonzalez-Urquijo et al. (3), 2019 | 5 | Two-stage urination [2], abdominal pain [2], MOF [1] | No | Pre-op | CT scan [3], US and cystography [2]‡ | Open | None | No (28) |
| Cimadamore et al. (7), 2019 | 1 | Hematuria | No | Pre-op | CT scan | Open | None | N/A |
| Wang et al. (8), 2018 |
1 | Two-stage urination | No | Pre-op | CT scan and cystography | Open | None | No [24] |
| Safavy et al. (9), 2018 | 1 | Flank and groin pain, hematuria, AKI | No | Pre-op | CT scan, cystoscopy | Open | Hydronephrosis | No [4] |
| Ghielmini et al. (10), 2017 | 1 | Oliguria, AKI | No | Pre-op | CT scan | Open | None | No [6] |
| François et al. (11), 2017 | 1 | Urosepsis, AKI | No | Pre-op | CT scan | Open§ | None | No [1] |
| Ugur et al. (12), 2016 | 1 | Two-stage urination | No | Pre-op | CT scan | Open | None | N/A |
| Tokgöz et al. (13), 2016 | 1 | Flank pain, scrotal mass | No | Pre-op | CT scan | Open | None | N/A |
| Kim et al. (5), 2011 | 1 | Scrotal mass | Ipsilateral, open | Intra-op | None | Open | None | No [2] |
| Khan et al. (14), 2014 | 2 | Urinary frequency [1] | No | Pre-op | US and MRI | TAPP | Scrotal | No [6] |
| Urinary incontinence [1] | No | Pre-op | Cystogram | TAPP | hematoma | No [5] | ||
| Umemura et al. (15), 2018 | 1 | Urinary frequency, two-stage urination | Bilateral, TAPP | Pre-op | CT scan | TAPP | None | No (N/A) |
| Karanikas et al. (32), 2020 | 1 | AKI, Inguinoscrotal mass | No | Pre-op | US | Open | None | No (N/A) |
| Hasegawa et al. (16), 2021 | 32 | Urinary frequency [4], sensation of residual urine [1] | No | Pre-op | CT scan (prone position) | TEP | None | 1 of 32 patients [2] |
| Tazaki et al. (17), 2019 | 1 | Abdominal pain, vomiting, diarrhea | No | Pre-op | CT scan | TAPP | None | No [24] |
| Namba et al. (18), 2020 | 1 | Urinary frequency, inguinal mass | No | Pre-op | CT scan | TAPP | None | N/A |
| Lee et al. (19), 2013 | 1 | Two-stage urination, inguinoscrotal mass | No | Pre-op | US, CT scan, cystography | TAPP | None | N/A |
| Kohga et al. (20), 2021 | 1 | Inguinal mass | No | Pre-op | CT scan | TAPP | None | No [2] |
| Chang et al. (21), 2021 | 1 | Urinary frequency, urosepsis, AKI, inguinoscrotal mass | No | Pre-op | CT scan | TEP | None | N/A |
| AlMohaya et al. (22), 2019 | 1 | Urinary frequency, hesitancy | Ipsilateral, TAPP | Pre-op | CT scan | Open | None | No [1] |
| Moufid et al. (23), 2013 | 4 | Inguinoscrotal mass [1] | Ipsilateral, open | Pre-op | Cystography | Open | None | N/A |
| Two-stage urination [1] | No | Pre-op | Cystography | Open | None | No [1] | ||
| Inguinal mass [1] | No | Intra-op | Methylene blue bladder instillation | Open | Bladder injury | N/A | ||
| Inguinal mass, urinary incontinence [1] | Ipsilateral, open | Post-op | Exploratory laparotomy | Open | Bladder injury, intraabdominal bleeding | No [12] | ||
| Omari et al. (24), 2013 | 1 | Two-stage urination, urinary frequency, urgency | No | Pre-op | US, cystography | Open: femoral, inguinal | None | No [6] |
| Katsourakis et al. (25), 2014 | 1 | Inguinal mass, bladder tumor | Contralateral, open | Pre-op | CT scan | Open | None | No [12] |
| Westera et al. (26), 2012 | 1 | Two-stage urination, inguinoscrotal mass | No | Pre-op | US, MRI | Open | None | N/A |
| Ellimoottil et al. (27), 2012 | 1 | AKI, Urinary frequency | No | Pre-op | CT cystography | Open | None | N/A |
| Tarchouli et al. (35), 2015 | 1 | Giant inguinoscrotal mass, difficult urination | No | Pre-op | CT scan | Open | None | No [6] |
| McKay et al. (30), 2014 | 1 | Two-stage urination, Inguinoscrotal mass | No | Pre-op | CT scan | Open, transperitoneal | Bladder ischemia, UTI | N/A |
| Coelho et al. (33), 2016 | 1 | AKI | No | Pre-op | Antegrade nephrostography, cystography | Open | None | N/A |
| Karatzas et al. (28), 2013 | 1 | Two-stage urination, CRF, urinary frequency, inguinoscrotal mass | No | Pre-op | US, CT scan | Open | None | No [6] |
| Frenkel et al. (31), 2015 | 1 | Two-stage urination, urinary retention | No | Pre-op | CT scan | Open | None | No [24] |
| Uchio et al. (29), 2012 | 1 | Urinary frequency, UTI, Inguinal mass | No | Pre-op | Pyelogram, cystoscopy, cystography | TAPP | None | No [24] |
| Ryan et al. (34), 2015 | 1 | Urinary retention, AKI | No | Pre-op | CT scan | Trans-scrotal cystostomy | None | N/A |
| Present report | 2 | Inguinoscrotal mass [1] | No | Intra-op | Bladder insufflation | Open | None | No [7] |
| Recurrence hernia [1] | Ipsilateral, open | Post-op | eTEP | No [6] |
†, parenthesis indicates number of patients; ‡, outcomes at the last follow-up; §, two-step approach: open repair after laparoscopic reduction. Pre-op, pre-operation; CT, computed tomography; N/A, not available; AKI, acute kidney injury; ESRD, end-stage kidney disease; MOF, multiorgan failure; US, ultrasonography; Intra-op, intra-operation; eTEP, extended-totally extraperitoneal; TAPP, transabdominal preperitoneal; MRI, magnetic resonance imaging; UTI, urinary tract infection; CRF, chronic renal failure.
Table 2
| Symptoms or signs of inguinal bladder hernia |
| Urinary frequency |
| Two-stage urination |
| Acute kidney injury |
| Abdominal or flank or scrotal pain |
| Hematuria |
| Urinary retention |
| Inguinoscrotal mass |
| Urinary tract infection |
| Oliguria |
| Urinary incontinence |
| Hesitancy or difficult urination |
| Sensation of residual urine |
Discussion
This present study has added two new cases of IBH to the body of literature; moreover, this report includes the first case of a laparoscopic eTEP approach for treatment of IBH. Open hernioplasty may result in recurrence, if the hernia is extraperitoneal bladder type with herniated through the pubic tubercle area. Hence, a laparoscopic approach seems to be superior to an open repair; in terms of diagnosis and repair of extraperitoneal IBH.
Regarding diagnosis of IBH, when patients have one or more of the following signs/symptoms: urinary frequency, two-stage urination, AKI in combination with an inguinoscrotal mass, in this clinical setting it is highly suggestive of IBH (2,3,6-12,15,16). CT scanning is the imaging of choice in such cases (2-4,6-13,15,17-22,25,27,28,30,31,35). Although, our second patient had abnormal urinary symptoms, the diagnosis of IBH was still missed during pre-operative and intra-operative of open hernioplasty. We revealed that the missed diagnosis of IBH was attributed to the location of the herniated bladder through the pubic tubercle area corresponding to the superficial inguinal ring. During open hernioplasty, this area is usually not covered by mesh; thus, the IBHs could be missed during surgery. This is consistent with reported series with history of ipsilateral open hernioplasty (4-6,22,23). This patient had an incarcerated hernia with suspected SBO that necessitated emergency surgery, so, preoperative CT scan was not performed. The early diagnosis of IBH is of paramount importance, as AKI, MOF and end-stage renal disease are the results of delayed diagnosis (2,3). We found that, if IBH is suspected during an operation, insufflation of the bladder, via a Foley’s catheter, is both a simple and valid tool for diagnosis.
In cases of preoperatively diagnosed IBH, either an open or laparoscopic approach can be used. However, laparoscopy has a number of advantages over an open procedure; including, shorter hospital stay, an earlier resume to daily activities, better cosmetic results, and equally low or reduced complication rates, are indeed a few of the benefits (36). In addition, TEP approach had been the preferred approach in extraperitoneal type of IBH compared to intraperitoneal and paraperitoneal type. Regarding IBHs in whom preoperative diagnosis could not be made or were recurrent after an anterior approach, we found that a laparoscopic eTEP approach offers clearer visibility of the hernia defect and content, avoids surgery in distorted anatomy or dense fibrous scarring. Moreover, wider operative field attributed to eTEP might be more suitable in an incarcerated case than TEP. Hence, laparoscopic eTEP would contribute to increased diagnostic yield, and a decreased chance of bladder injury. Furthermore, evidence has shown that an anterior approach has more pubic tubercle recurrence than a posterior approach (37). The extraperitoneal posterior mesh placement ensures the covering of all potential defects (37); including, more medially, and the pubic tubercle or extraperitoneal type of IBH (16).
Conclusions
IBH is a rare disease, and prompt diagnosis should be made in patients presenting with an inguinoscrotal mass along with urinary frequency, two-stage urination, AKI. Bladder insufflation is a simply tool for intraoperative diagnosis. Additionally, Laparoscopic eTEP repair might offer advantages of diagnosis and repairing of incarcerated extraperitoneal type of IBH.
Acknowledgments
The authors would like to thank Mr. Andrew Jonathan Tait for his assistant in English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-21-19/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-21-19/coif). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (approval No. REC.64-406-10-3) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tanoue K, Okino H, Kanazawa M, et al. Single-incision laparoscopic transabdominal preperitoneal mesh hernioplasty: results in 182 Japanese patients. Hernia 2016;20:797-803. [Crossref] [PubMed]
- Levi J, Chopra K, Hussain M, et al. Rare giant inguinal hernia causing end-stage dialysis-dependent renal failure. BMJ Case Rep 2020;13:233140. [Crossref] [PubMed]
- Gonzalez-Urquijo M, Mayagoitia-Gonzalez JC, Rodarte-Shade M, et al. Large inguinal bladder hernias: can a preoperative diagnosis be made? Hernia 2019;23:1221-7. [Crossref] [PubMed]
- Bernhardson ND, Shepherd MH, Shermer CD. Massive bladder inguinal hernia leading to acute urinary retention. Am J Emerg Med 2021;39:253.e3-5. [Crossref] [PubMed]
- Kim KH, Kim MU, Jeong WJ, et al. Incidentally detected inguinoscrotal bladder hernia. Korean J Urol 2011;52:71-3. [Crossref] [PubMed]
- Tome J, Neidert N, Szostek J. Inguinoscrotal Bladder Hernia Causing Hydroureteronephrosis and Acute Kidney Injury. Mayo Clin Proc 2021;96:18-9. [Crossref] [PubMed]
- Cimadamore A, Palagonia E, Piccinni P, et al. Inguinal bladder hernia with lipomatosis of the bladder wall: A potential clinical pitfall for cancer. Urologia 2019;86:35-8. [Crossref] [PubMed]
- Wang P, Huang Y, Ye J, et al. Large sliding inguino-scrotal hernia of the urinary bladder: A case report and literature review. Medicine (Baltimore) 2018;97:e9998. [Crossref] [PubMed]
- Safavy S, Mitsinikos E, Tropea B, et al. Obstructive Uropathy and Sepsis Caused by an Inguinoscrotal Bladder Hernia: A Case Report. Perm J 2018;22:17-052. [Crossref] [PubMed]
- Ghielmini E, Julita L, Cerantola Y, et al. Inguinal Bladder Hernia With Acute Ureteral Obstruction 14 Years After Kidney Transplantation: A Case Report. Transplant Proc 2017;49:1593-5. [Crossref] [PubMed]
- François J, Defoort B, Muysoms F. Complicated inguino-scrotal bladder hernia: a case of two-step repair. Acta Chir Belg 2017;117:122-4. [Crossref] [PubMed]
- Ugur M, Atcı N, Oruc C, et al. Left Inguinal Bladder Hernia that Causes Dilatation in the Ureter. Arch Iran Med 2016;19:376-8. [PubMed]
- Tokgöz H, Tokgöz Ö, Karamık K, et al. Pathological changes in herniated organs: squamous metaplasia in an inguino-scrotal bladder hernia. Hernia 2016;20:891-2. [Crossref] [PubMed]
- Khan A, Beckley I, Dobbins B, et al. Laparoscopic repair of massive inguinal hernia containing the urinary bladder. Urol Ann 2014;6:159-62. [Crossref] [PubMed]
- Umemura A, Suto T, Fujuwara H, et al. Laparoscopic Repair for Recurrent Bilateral Inguinal Bladder Hernia following Bilateral Transabdominal Preperitoneal Repair. Case Rep Surg 2018;2018:4904093. [Crossref] [PubMed]
- Hasegawa S, Ogino N, Kanemura T, et al. Clinical characteristics of inguinal bladder hernias and total extraperitoneal repair. Asian J Endosc Surg 2021;14:394-400. [Crossref] [PubMed]
- Tazaki T, Sasaki M, Kohyama M, et al. Inguinoscrotal hernia containing the urinary bladder successfully repaired using laparoscopic transabdominal preperitoneal repair technique: A case report. Asian J Endosc Surg 2019;12:201-3. [Crossref] [PubMed]
- Namba Y, Fukuda T, Ishikawa S, et al. Inguinal bladder hernia treated using transabdominal preperitoneal approach: A case report. Int J Surg Case Rep 2020;67:165-8. [Crossref] [PubMed]
- Lee JY, Oh SY, Chang IH, et al. Laparoscopic repair of large bladder herniation presenting as an inguinal hernia. Korean J Urol 2013;54:139-42. [Crossref] [PubMed]
- Kohga A, Okumura T, Yamashita K, et al. A case of indirect inguinal bladder hernia treated by laparoscopic hernia repair. Asian J Endosc Surg 2021;14:128-31. [Crossref] [PubMed]
- Chang HH, Wen SC. Extraperitoneal laparoscopic repair of huge inguinoscrotal bladder hernia: A case report and literature review. Urol Case Rep 2021;38:101735. [Crossref] [PubMed]
- AlMohaya N, Alabdrabalameer MNE, AlAnazi K, et al. Bilateral inguinal bladder hernia following unilateral transabdominal preperitoneal repair. A case report and review of the literature. Ann Med Surg (Lond) 2019;46:23-6. [Crossref] [PubMed]
- Moufid K, Touiti D, Mohamed L. Inguinal bladder hernia: four case analyses. Rev Urol 2013;15:32-6. [PubMed]
- Omari AH, Alghazo MA. Urinary bladder diverticulum as a content of femoral hernia: a case report and review of literature. World J Emerg Surg 2013;8:20. [Crossref] [PubMed]
- Katsourakis A, Noussios G, Svoronos C, et al. Direct inguinal hernia containing bladder carcinoma: A case report and review of the literature. Int J Surg Case Rep 2014;5:180-2. [Crossref] [PubMed]
- Westera J, Meyer J, Reynolds J, et al. Massive inguinoscrotal bladder hernia. J Surg Case Rep 2012;2012:5. [Crossref] [PubMed]
- Ellimoottil C, Ross M, Hart ST, et al. Unusual videourodynamic finding: massive scrotal cystocele. Urology 2012;80:e53-4. [Crossref] [PubMed]
- Karatzas A, Christodoulidis G, Spyridakis M, et al. A giant inguinoscrotal bladder hernia as a cause of chronic renal failure: A rare case. Int J Surg Case Rep 2013;4:345-7. [Crossref] [PubMed]
- Uchio EM, Calderon JS, Hwang JJ. Laparoscopic repair of inguinal cystocele using cystoscopic light test. Urology 2012;79:725-7. [Crossref] [PubMed]
- McKay JP, Organ M, Bagnell S, et al. Inguinoscrotal hernias involving urologic organs: A case series. Can Urol Assoc J 2014;8:E429-32. [Crossref] [PubMed]
- Frenkel A, Roy-Shapira A, Shelef I, et al. Inguinal Herniation of the Urinary Bladder Presenting as Recurrent Urinary Retention. Case Rep Surg 2015;2015:531021. [Crossref] [PubMed]
- Karanikas M, Kofina K, Foutzitzi S, et al. Urinary bladder-containing incarcerated inguinoscrotal hernia: a case report. J Surg Case Rep 2020;2020:rjaa092.
- Coelho H, Nunes P, Canhoto C, et al. Inguinal hernia containing bladder and ureteroneocystostomy: a rare cause for acute renal graft dysfunction. BMJ Case Rep 2016;2016:bcr2016214466. [Crossref] [PubMed]
- Ryan ST, Jumper B. Scrotal Cystocele Managed With Trans-scrotal Neocystostomy Tube. Urol Case Rep 2015;3:117-9. [Crossref] [PubMed]
- Tarchouli M, Ratbi MB, Bouzroud M, et al. Giant inguinoscrotal hernia containing intestinal segments and urinary bladder successfully repaired by simple hernioplasty technique: a case report. J Med Case Rep 2015;9:276. [Crossref] [PubMed]
- EU Hernia Trialists Collaboration. Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 2000;87:860-7. [PubMed]
- Saber A, Ellabban GM, Gad MA, et al. Open preperitoneal versus anterior approach for recurrent inguinal hernia: a randomized study. BMC Surg 2012;12:22. [Crossref] [PubMed]
Cite this article as: Rachiwong L, Wiboonkhwan NA, Cheewatanakornkul S. Advantages of minimally invasive approach for inguinal bladder hernia repair: case report and literature review. Laparosc Surg 2022;6:8.


