
Results after minimally invasive Toupet fundoplication technique: a narrative review
Introduction
Laparoscopic fundoplication is considered the standard surgical treatment for patients with gastro-esophageal reflux disease (GERD). It determines excellent control of symptoms both at short and long-term follow-up (1,2). However, laparoscopic fundoplication is associated with the presence of side-effect, mainly new onset of dysphagia and gas-bloat syndrome (3).
Posterior partial fundoplication (PPF) was described by Andrè Toupet as an open procedure in 1963, in attempt to reduce the rate of dysphagia and gas bloat syndrome that occurred after Nissen fundoplication (4). The operation was performed through a midline incision, and the original technique described a partial wrap of the gastric fundus behind the mobilized esophagus without short gastric vessels division. This technique initially proposed as a 180° posterior wrap, and subsequently modified to a 270° wrap, did not originally include a hiatoplasty except in case of very enlarged hiatus.
Proponents of the Toupet technique argue that, allowing patients to vent air from the stomach, PPF could result in minor mechanical disadvantages in comparison to total fundoplication, without losing efficacy on reflux control (5).
With the advent of laparoscopy and the recognition of its advantages over the open approach, this technique has been translated into minimally invasive surgery (6). However, data specifically assessing the comparison between open and laparoscopic posterior partial fundoplication (LPPF) are scarce. Only Hakanson et al. reported the results of a randomized controlled trial comparing 93 patients submitted to open and 99 patients to LPPF (7). This study showed that complication rates and length of stay were higher in the open group, while at medium-term follow-up (3 years) there were no differences in terms of reflux control, use of medications and overall patients’ satisfaction between the two groups. For these reasons, laparoscopic surgery was considered the treatment of choice.
The aim of this paper is to provide a narrative review the literature on the results of minimally invasive Toupet fundoplication technique. We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/ls-20-101).
Surgical technique
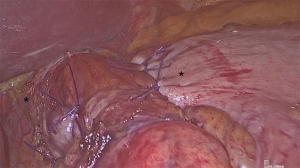
The procedure can be formed laparoscopically or with the robotic approach (8). When performed laparoscopically, five trocars are needed; when performed with the DaVinci Xi Surgical System (Intuitive Surgical Inc., Sunnyvale, CA, USA) four robotic trocars are introduced, and two additional laparoscopic trocars are placed for exposure. Operative steps are the same either with the laparoscopic and the robotic approach. The first step of the procedure is the exposure of the esophageal hiatus: the right and left diaphragmatic crura are visualized and the posterior aspect of the esophagus is dissected in order to create a retroesophageal window. A vessel loop is passed around the esophagus to provide inferior traction, helping esophageal mobilization, until at least 2–3 cm of the lower esophagus remain in abdomen without tension. At this point the gastric fundus can be pulled behind the esophagus to the right of the patient, without short gastric vessel division. A hiatoplasty with interrupted stitches is required. The gastric fundus is then anchored to the right and to the left aspects of the esophagus with interrupted stitches (Figure 1). Furthermore, some authors propose to anchor the gastric wrap to the crura, as described in the original Toupet technique (4).
Postoperative care
The nasogastric tube is removed at the end of the surgical procedure, except in the case of a concurrent large paraesophageal hernia repair. On the first postoperative day patients are allowed to start with clear liquids, while soft meal is introduced the day after. The discharge generally takes place on second postoperative day. Patients are instructed to a detailed diet with semi-solid foods for at least 30 days (9,10).
Short- and medium-term results
Several studies have evaluated the short-term outcomes of LPPF, demonstrating safety, feasibility and effectiveness of the procedure (Table 1) (11-17).
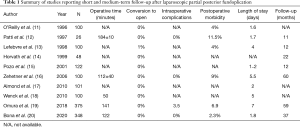
Full table
More recently, the medium-term results of series of LPPF were published. For instance, Omura et al. described the results of 375 patients undergoing laparoscopic Toupet fundoplication between 1997 and 2016. Clinical recurrence of symptoms was experienced in 15.1% of cases. Patients were therefore divided into 2 groups based on the presence of GERD recurrence. The authors concluded that longer preoperative acid reflux time, the presence of hiatal hernia, and the severity of reflux esophagitis were predictive factors of recurrence after LPPF (19).
Also, Bona et al. performed a medium-term analysis on 348 GERD patients submitted to LPPF. A bio-synthetic mesh was added for crural augmentation in 177 (51%) patients. At a mean follow-up of 37 months, 95% of patients was satisfied about the procedure, with only 1.1% patients complaining of persistent dysphagia (20).
The results of 5-year follow-up of 100 consecutive LPPF patients was published by Zehether et al. The rate of endoscopic dilatation for persistent dysphagia was 5% after 12 months from the surgical procedure. At 5 years follow-up, overall satisfaction was 96.3%. Clinical GERD recurrence occurred in 15% of patients, while occasional dysphagia was present in 2% of patients (16).
Long term results
Long term results (>10 years) of LPPF are scarce. Dallemagne et al. reported the long-term follow up results of a prospective observational study comparing laparoscopic total (68 patients) vs. LPPF (32 patients). At 10-year follow-up patients were investigated with a structured symptom questionnaire, showing that 81.8% of patients submitted to LPPF were free from GERD symptoms and occasional postoperative dysphagia was experienced in 25% of patients (21).
The only study specifically assessing long-term results of Toupet fundoplication is the one performed by Franzen et al., with the open approach. They described the long-term results of 101 patients submitted to open PPF between 1982 and 1989. At 10 years after surgery, recurrence rate was 8%, and patients with severe preoperative esophagitis were at higher risk of developing recurrence. Therefore the authors concluded that in severe GERD patients Toupet fundoplication was not indicated (22).
Toupet vs. Nissen
In the last two decades, several RCTs compared LPPF and Nissen fundoplication, showing minimal differences between the two procedures (23-26). Furthermore, various meta-analysis were conducted to clarify which was the best surgical procedure for GERD (27-32). These studies agreed in the description of LPPF as the procedure that guarantees the best balance between reflux control and side-effects. For instance, in a recent network meta-analysis including 29 RCTs that compared different laparoscopic anti-reflux procedures, Andreou et al. concluded that Toupet fundoplication was equally effective as Nissen fundoplication in reflux control, morbidity and reoperations, while it was associated with lower dysphagia and gas-bloat syndrome (33).
However, the reliability and accuracy of the results of these meta-analyses are limited, due to the extreme heterogeneity between the studies regarding the methodological quality of the included studies, preoperative indications, patients baseline characteristics, and surgical technique performed (200–270° degree of partial wrap, use of a bougie, crural repair, short gastric vessel division, length of the fundoplication, inclusion of open procedures). Furthermore, the duration of follow-up, that was less than 5 years in the majority of included studies, cannot allow to draw definitive conclusions on long-term effectiveness of the procedures.
In the 1990’s, in the debate between total and partial fundoplication, the so called “tailored approach” came into vogue. Some studies showed that the postoperative functional results appeared to be better after LPPF, particularly in the subgroup of GERD patients with esophageal dismotility (34,35). Therefore, some authors proposed to select for Toupet fundoplication patients who were at higher risk of developing postoperative dysphagia after Nissen fundoplication, such as patients with impaired peristalsis (36).
However, subsequent RCTs aiming to clarify the best procedure between LPPF and Nissen fundoplication for patients with impaired peristalsis, did not confirm these results (12,14,37-39). Therefore, this approach, of tailoring degree of fundoplication based on results of preoperative esophageal motility studies, has been abandoned.
One of the main claims against Toupet fundoplication is the uncertainty regarding the maintenance of its effects over time. In fact, some authors reported poorer reflux control after LPPF than Nissen fundoplication at long-term follow-up, and it seems that the mechanical advantages of Toupet fundoplication tend to disappear with time (12,32,40-43).
Toupet vs. anterior partial
After the description of posterior partial 180° fundoplication by Toupet, further modifications of the original Nissen fundoplication, in an attempt to find the best procedure capable of ensuring lower side effects maintaining reflux control, led to the development of anterior partial fundoplications.
Laparoscopic anterior partial fundoplications (LAPF) were associated to fewer side effects than Nissen fundoplication. Broeders et al., analyzing the raw data set of 4 RCTs comparing Nissen and LAPF, demonstrated that at 5 years of follow-up, reflux control was similar between Nissen an 180° LAPF, but lower after 90° LAPF. The authors concluded that the results supported the use of 180° LAPF in the surgical treatment of GERD (44).
Several studies aiming to compare LAPF vs. LPPF were performed (45,46). For instance, Roks et al. performed a two-center double-blind RCT comparing laparoscopic Toupet and 180° LAPF (47 patients in each group). No differences between the two procedures in the rate of postoperative dysphagia and in reflux control were detected at 1 year follow-up (47).
Also, Daud et al. performed a multicenter RCT comparing 180° LAPF (23 patients) and LPPF (24 patients). The results were inconclusive, but a trend towards higher reflux symptoms and pH score after LAPF was present already 12 months after surgery (48).
However, small sample sizes and short-term follow up of studies comparing LAPF and LPPF partial fundoplication could not draw definitive conclusions on the role of anterior partial fundoplication.
Conclusions
Since the first description of posterior partial fundoplication by Andre Toupet in 1963, this procedure has gained wide acceptance. Safety and feasibility of this procedure performed with minimally invasive approach have been demonstrated by several series. The short- and medium-term results of RCTs showed similar reflux control compared to Nissen fundoplication, with lower side effects. However, long term data are lacking and the durability of Toupet procedure over time is questioned. Therefore, the debate on which should be considered the best anti-reflux procedure in the surgical management of GERD, remains open.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Andrea Balla) for the series “Minimally Invasive Approach for the Treatment of Gastro-esophageal Reflux Disease” published in Laparoscopic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/ls-20-101
Peer Review File: Available at http://dx.doi.org/10.21037/ls-20-101
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls-20-101). The series “Minimally Invasive Approach for the Treatment of Gastro-esophageal Reflux Disease” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fuchs KH, Feussner H, Bonavina L, et al. Current status and trends in laparoscopic antireflux surgery: results of a consensus meeting. The European Study Group for Antireflux Surgery (ESGARS). Endoscopy 1997;29:298-308. [Crossref] [PubMed]
- Stefanidis D, Hope WW, Kohn GP, et al. Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc 2010;24:2647-69. [Crossref] [PubMed]
- Richter JE. Gastroesophageal reflux disease treatment: side effects and complications of fundoplication. Clin Gastroenterol Hepatol 2013;11:465-71. [Crossref] [PubMed]
- Toupet A. Technic of esophago-gastroplasty with phrenogastropexy used in radical treatment of hiatal hernias as a supplement to Heller’s operation in cardiospasms. Mem Acad Chir (Paris) 1963;89:384-9. [PubMed]
- Watson A, Jenkinson LR, Ball CS, et al. A more physiological alternative to total fundoplication for the surgical correction of resistant gastro-oesophageal reflux. Br J Surg 1991;78:1088-94. [Crossref] [PubMed]
- Peters MJ, Mukhtar A, Yunus RM, et al. Meta-analysis of randomized clinical trials comparing open and laparoscopic anti-reflux surgery. Am J Gastroenterol 1562;2009:1548-61. [PubMed]
- Håkanson BS, Thor KBA, Thorell A, et al. Open vs laparoscopic partial posterior fundoplication. A prospective randomized trial. Surg Endosc 2007;21:289-98. [Crossref] [PubMed]
- Wykypiel H, Wetscher GJ, Klaus A, et al. Robot-assisted laparoscopic partial posterior fundoplication with the DaVinci system: initial experiences and technical aspects. Langenbecks Arch Surg 2003;387:411-6. [Crossref] [PubMed]
- Rebecchi F, Allaix ME, Giaccone C, et al. Gastric emptying as a prognostic factor for long-term results of total laparoscopic fundoplication for weakly acidic or mixed reflux. Ann Surg 2013;258:831-6; discussion 836-837. [Crossref] [PubMed]
- Morino M, Pellegrino L, Giaccone C, et al. Randomized clinical trial of robot-assisted versus laparoscopic Nissen fundoplication. Br J Surg 2006;93:553-8. [Crossref] [PubMed]
- O’Reilly MJ, Mullins SG, Saye WB, et al. Laparoscopic posterior partial fundoplication: analysis of 100 consecutive cases. J Laparoendosc Surg 1996;6:141-50. [Crossref] [PubMed]
- Patti MG, Robinson T, Galvani C, et al. Total fundoplication is superior to partial fundoplication even when esophageal peristalsis is weak. J Am Coll Surg 2004;198:863-9; discussion 869-870. [Crossref] [PubMed]
- Lefebvre JC, Belva P, Takieddine M, et al. Laparoscopic Toupet fundoplication: prospective study of 100 cases. Results at one year and literature review. Acta Chir Belg 1998;98:1-4. [Crossref] [PubMed]
- Horvath KD, Jobe BA, Herron DM, et al. Laparoscopic Toupet fundoplication is an inadequate procedure for patients with severe reflux disease. J Gastrointest Surg 1999;3:583-91. [Crossref] [PubMed]
- Pozo F, Giganto F, Rodrigo L. Clinical efficacy of the Toupet technique performed by laparoscopic surgery. Medium-term follow-up in 122 cases. Surg Endosc 2001;15:1171-4. [Crossref] [PubMed]
- Zehetner J, Holzinger F, Breuhahn T, et al. Five-year results of laparoscopic Toupet fundoplication as the primary surgical repair in GERD patients: is it durable? Surg Endosc 2006;20:220-5. [Crossref] [PubMed]
- Almond LM, Wadley MS. A 5-year prospective review of posterior partial fundoplication in the management of gastroesophageal reflux disease. Int J Surg 2010;8:239-42. [Crossref] [PubMed]
- Wenck C, Zornig C. Laparoscopic Toupet fundoplication. Langenbecks Arch Surg 2010;395:459-61. [Crossref] [PubMed]
- Omura N, Yano F, Tsuboi K, et al. Surgical results of laparoscopic Toupet fundoplication for gastroesophageal reflux disease with special reference to recurrence. Esophagus 2018;15:217-23. [Crossref] [PubMed]
- Bona D, Aiolfi A, Asti E, et al. Laparoscopic Toupet fundoplication for gastroesophageal reflux disease and hiatus hernia: proposal for standardization using the ‘critical view’ concept. Updates Surg 2020;72:555-8. [Crossref] [PubMed]
- Dallemagne B, Weerts J, Markiewicz S, et al. Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 2006;20:159-65. [Crossref] [PubMed]
- Franzén T, Boström J, Tibbling Grahn L, et al. Prospective study of symptoms and gastro-oesophageal reflux 10 years after posterior partial fundoplication. Br J Surg 1999;86:956-60. [Crossref] [PubMed]
- Håkanson BS, Lundell L, Bylund A, et al. Comparison of Laparoscopic 270° Posterior Partial Fundoplication vs Total Fundoplication for the Treatment of Gastroesophageal Reflux Disease: A Randomized Clinical Trial. JAMA Surg 2019;154:479-86. [Crossref] [PubMed]
- Qin M, Ding G, Yang H. A clinical comparison of laparoscopic Nissen and Toupet fundoplication for gastroesophageal reflux disease. J Laparoendosc Adv Surg Tech A 2013;23:601-4. [Crossref] [PubMed]
- Koch OO, Kaindlstorfer A, Antoniou SA, et al. Comparison of results from a randomized trial 1 year after laparoscopic Nissen and Toupet fundoplications. Surg Endosc 2013;27:2383-90. [Crossref] [PubMed]
- Wang B, Zhang W, Liu S, et al. A Chinese randomized prospective trial of floppy Nissen and Toupet fundoplication for gastroesophageal disease. Int J Surg 2015;23:35-40. [Crossref] [PubMed]
- Amer MA, Smith MD, Khoo CH, et al. Network meta-analysis of surgical management of gastro-oesophageal reflux disease in adults. Br J Surg 2018;105:1398-407. [Crossref] [PubMed]
- Broeders JA, Mauritz FA, Ahmed Ali U, et al. Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg 2010;97:1318-30. [Crossref] [PubMed]
- Shan C-X, Zhang W, Zheng X-M, et al. Evidence-based appraisal in laparoscopic Nissen and Toupet fundoplications for gastroesophageal reflux disease. World J Gastroenterol 2010;16:3063-71. [Crossref] [PubMed]
- Tan G, Yang Z, Wang Z. Meta-analysis of laparoscopic total (Nissen) versus posterior (Toupet) fundoplication for gastro-oesophageal reflux disease based on randomized clinical trials. ANZ J Surg 2011;81:246-52. [Crossref] [PubMed]
- Tian ZC, Wang B, Shan CX, et al. A Meta-Analysis of Randomized Controlled Trials to Compare Long-Term Outcomes of Nissen and Toupet Fundoplication for Gastroesophageal Reflux Disease. PLoS One 2015;10:e0127627. [Crossref] [PubMed]
- Du X, Hu Z, Yan C, et al. A meta-analysis of long follow-up outcomes of laparoscopic Nissen (total) versus Toupet (270°) fundoplication for gastro-esophageal reflux disease based on randomized controlled trials in adults. BMC Gastroenterol 2016;16:88. [Crossref] [PubMed]
- Andreou A, Watson DI, Mavridis D, et al. Assessing the efficacy and safety of laparoscopic antireflux procedures for the management of gastroesophageal reflux disease: a systematic review with network meta-analysis. Surg Endosc 2020;34:510-20. [Crossref] [PubMed]
- Gunter RL, Shada AL, Funk LM, et al. Long-Term Quality of Life Outcomes Following Nissen Versus Toupet Fundoplication in Patients with Gastroesophageal Reflux Disease. J Laparoendosc Adv Surg Tech A 2017;27:931-6. [Crossref] [PubMed]
- Jobe BA, Wallace J, Hansen PD, et al. Evaluation of laparoscopic Toupet fundoplication as a primary repair for all patients with medically resistant gastroesophageal reflux. Surg Endosc 1997;11:1080-3. [Crossref] [PubMed]
- Fernando HC, Luketich JD, Christie NA, et al. Outcomes of laparoscopic Toupet compared to laparoscopic Nissen fundoplication. Surg Endosc 2002;16:905-8. [Crossref] [PubMed]
- Mardani J, Lundell L, Engström C. Total or posterior partial fundoplication in the treatment of GERD: results of a randomized trial after 2 decades of follow-up. Ann Surg 2011;253:875-8. [Crossref] [PubMed]
- Lund RJ, Wetcher GJ, Raiser F, et al. Laparoscopic Toupet fundoplication for gastroesophageal reflux disease with poor esophageal body motility. J Gastrointest Surg 1997;1:301-8; discussion 308. [Crossref] [PubMed]
- Patti MG, De Pinto M, de Bellis M, et al. Comparison of laparoscopic total and partial fundoplication for gastroesophageal reflux. J Gastrointest Surg 1997;1:309-14; discussion 314-315. [Crossref] [PubMed]
- Kauer WK, Peters JH, DeMeester TR, et al. A tailored approach to antireflux surgery. J Thorac Cardiovasc Surg 1995;110:141-6; discussion 146-147. [Crossref] [PubMed]
- Fibbe C, Layer P, Keller J, et al. Esophageal motility in reflux disease before and after fundoplication: a prospective, randomized, clinical, and manometric study. Gastroenterology 2001;121:5-14. [Crossref] [PubMed]
- Booth MI, Stratford J, Jones L, et al. Randomized clinical trial of laparoscopic total (Nissen) versus posterior partial (Toupet) fundoplication for gastro-oesophageal reflux disease based on preoperative oesophageal manometry. Br J Surg 2008;95:57-63. [Crossref] [PubMed]
- Zornig C, Strate U, Fibbe C, et al. Nissen vs Toupet laparoscopic fundoplication. Surg Endosc 2002;16:758-66. [Crossref] [PubMed]
- Broeders JA, Roks DJ, Jamieson GG, et al. Five-year outcome after laparoscopic anterior partial versus Nissen fundoplication: four randomized trials. Ann Surg 2012;255:637-42. [Crossref] [PubMed]
- Oor JE, Broeders JA, Roks DJ, et al. Reflux and Belching after Laparoscopic 270 degree Posterior Versus 180 degree Anterior Partial Fundoplication. J Gastrointest Surg 2018;22:1852-60. [Crossref] [PubMed]
- Engström C, Ruth M, Lönroth H, et al. Manometric characteristics of the gastroesophageal junction after anterior versus posterior partial fundoplication. Dis Esophagus 2005;18:31-6. [Crossref] [PubMed]
- Roks DJ, Koetje JH, Oor JE, et al. Randomized clinical trial of 270° posterior versus 180° anterior partial laparoscopic fundoplication for gastro-oesophageal reflux disease. Br J Surg 2017;104:843-51. [Crossref] [PubMed]
- Daud WNW, Thompson SK, Jamieson GG, et al. Randomized controlled trial of laparoscopic anterior 180° partial versus posterior 270° partial fundoplication. ANZ J Surg 2015;85:668-72. [Crossref] [PubMed]
Cite this article as: Ugliono E, Seno E, Allaix ME, Rebecchi F, Morino M. Results after minimally invasive Toupet fundoplication technique: a narrative review. Laparosc Surg 2021;5:5.


