
Minimally invasive liver resections for hilar cholangiocarcinoma: a narrative review
Introduction
Radical resection is the only curative option among treatments for hilar cholangiocarcinoma (1-3). The main factors influencing the type of surgery are the longitudinal diffusion along the biliary tree and the radial extension toward the hilar structures and the liver parenchyma (4). Although an extrahepatic bile duct resection with locoregional lymphadenectomy is adequate for Bismuth type I tumours, the most acknowledged care for type II–IV contemplates also a liver resection: major hepatectomy and/or caudatectomy (named also caudate lobectomy) are highly recommended to enhance radicality (5-8). Whereas vascular resections are only performed for selected advanced cases, bilioenteric reconstruction is always needed and recognized a major source of morbidity for this surgery (9,10).
Minimally-invasive approaches, such as pure laparoscopy and robotic, have spread over the last 20 years in abdominal surgery, including liver and biliary tract operations (11-22). In this field, the treatment of bile duct tumours represents one of the last areas of resistance to their application. The reasons are the need of accurate assessment of resectability, meticulous lymphadenectomy en bloc with the peri-hilar tissues, and complex liver resection in a not negligible proportion of cases. Despite each of these procedures is demonstrated feasible by minimally-invasive techniques, surgery for hilar cholangiocarcinoma requires their combination in one single operation (23-27). As such, laparoscopic surgery for these patients demands substantial experience and advanced technical skills in both hepatobiliary and minimally-invasive surgery.
The aim of this review is to summarize the available evidence on minimally-invasiveness applied to the surgical treatment of hilar cholangiocarcinoma, focusing on the issues pertaining to pure laparoscopic or robotic liver resection. The final goal is to draw some considerations on its applicability, efficacy and diffusion. We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/ls-20-95).
Review strategy
A literature search was performed in the PubMed database. The search words were (“Klatskin” OR “hilar cholangiocarcinoma”) AND (“laparoscopic” OR “minimally-invasive” OR “robotic” OR “robot-assisted”). Language restriction was applied to include only English literature, and references of the retrieved articles were scrutinized for additional relevant studies and checked for duplicates. Publications up to March 2020 were considered. The studies collected are summarized in Table 1.
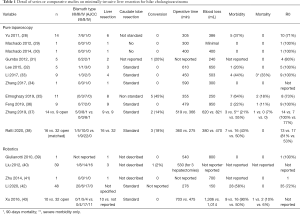
Full table
Pure laparoscopic resections
The first report on pure laparoscopic resections for hilar cholangiocarcinoma appeared in 2011 by Yu and colleagues (28). The authors reported on 14 patients approached laparoscopically between 2006 and 2008 at two Chinese institutions: 7 type I tumours were treated with bile duct resection and bilioenterical Roux-en-Y reconstruction, whereas 6 type II patients received concomitant partial liver resection as needed for involved liver segments (segment 1, 4 or 5). Patients without imaging suggesting vascular involvement nor liver atrophy were selected: the remaining 2 patients were discovered intraoperatively with more advanced tumours (portal vein invasion or Bismuth type IIIa) and underwent palliative bypass. All procedures were completed laparoscopically and in-hospital mortality was zero. Compared to Bismuth type I, procedures for Bismuth type II tumours had higher complication rate (60% vs. 14.7%), more frequent bile leak (60% vs. 14%), 2 port-site metastases and lower R0 resection rates (60% vs. 100%), explained by the non-standard resection of the caudate lobe. The authors concluded that laparoscopy can be an alternative to open surgery for selected Bismuth type I cholangiocarcinomas, whereas its adequacy for type II should undergo additional evaluation.
Following this research, only 8 small retrospective series were published between 2012 and 2019. All studies, except one, were based on single centre experiences, with a maximum of 9 patients reported.
In 2012, Machado and colleagues described the first laparoscopic major hepatectomy for Klatskin tumours (29). The patient received a laparoscopic left hemihepatectomy including lymphadenectomy and bile duct resection. The bilioenteric reconstruction on two small separate bile ducts was video-assisted through a small subcostal incision. Operative time was 5 hours, blood loss quantified as minimal without need for transfusions, postoperative course uneventful and length of stay 7 days. Final histology diagnosed a well-differentiated cholangiocarcinoma without nodal involvement and clear surgical margins. Two years later, the same group performed a totally laparoscopic right hemihepatectomy for a right-sided intraductal papillary mucinous neoplasm (30). The demolition phase included lymphadenectomy and biliary confluence resection. In this case, the bilioenteric anastomosis on a large biliary stump was totally laparoscopic, with a mechanical jejunojejunostomy and manual hepaticojejunostomy, whereas the specimen was extracted through a suprapubic incision. Operative time was 400 minutes, blood loss 400 mL without need for transfusions, postoperative course uneventful and length of stay 10 days. Negative margins on both the distal and left bile duct stump were achieved. In both publications, patients were free from disease recurrence at 18 and 14 months after the operation, respectively, and biliary stenosis was never documented. However, no caudate lobe resection nor the number of lymph nodes harvested was reported, despite the hilar lymphadenectomy was described as extensive. The authors concluded that laparoscopic approach is applicable for a safe left and right hepatectomy with lymphadenectomy for Klatskin tumours, and the use of a hybrid method may facilitate difficult biliary reconstructions; however, right hemihepatectomy should be attempted in specialized centres and selected patients. The authors stressed that progressive experience may decrease the long operative and postoperative times, as occurred with other surgeries.
In 2013, Gumbs and colleagues reported the laparoscopic experience of three international centres in treating 5 patients with extrapancreatic cholangiocarcinomas (31). One patient was converted because of suspected portal invasion, and 2 patients with Blumgart T2 lesions received concomitant left/right hemihepatectomy associated to the biliary resection and hepatoduodenal lymphadenectomy. The authors described the use of a periumbilical incision (± hand-port) for both specimen extraction and fashioning of the jejunojejunostomy, whereas the hepaticojejunostomy was performed laparoscopically. The patient receiving left hepatectomy had a final diagnosis of AJCC stage IV disease and R1 resection. No specific information was given regarding the intra and postoperative outcomes of the 2 patients treated with concomitant hepatectomy, nor on the number of nodes harvested or the caudate lobe resection. In view of their satisfactory results, the authors concluded that complex biliary reconstructions should not be considered a contraindication to laparoscopy, which might even be beneficial on the surgical technique for biliary reconstruction, and translate into less bile leaks.
Lee et al. also published their experience in 2015 (32). Five patients with hilar cholangiocarcinoma were treated with laparoscopic extrahepatic bile duct resection, and right/left hemihepatectomy for Bismuth type IIIa (1 patient) and type IIIb (2 patients) tumours. All liver resections were extended to caudate lobe, and hepatoduodenal lymphadenectomy was performed in all cases with a median of 4 nodes harvested. The bilioenteric anastomosis was fashioned using totally laparoscopic or laparoscopic-assisted technique via a small subcostal incision. The authors commented their results as favourable, comparable to other series and in support of the feasibility in selected patients, but also stressed the difficulty in selecting the most suitable cases.
Another report was published in 2017 by Li et al. (33). In this series 9 non-consecutive patients with Bismuth I-IV hilar cholangiocarcinoma were successfully operated by laparoscopy. Patients with lobe atrophy or vascular invasion at preoperative imaging were excluded from the laparoscopic approach. Four patients underwent concomitant liver resection, including isolated resection of the caudate lobe for Bismuth type II and left hepatectomy with caudatectomy for type IIIb. The authors highlighted that complete caudate lobectomy is easier when performed in combination to hepatectomy (as required for type III and IV type), since the access can be facilitated by the route of the left portal vein. In all cases, lymphadenectomy and en bloc resection of the hepatoduodenal tissues were part of the operation. For the bilioenteric anastomoses they used a totally laparoscopic approach for two cases, and hand-assisted technique or a small incision in the right upper quadrant for the remaining. The author suggestion was to consider a full laparoscopic approach for Bismuth I and II bilioenteric anastomosis (since the bile duct stump are one or two) and hand-assisted or direct visualization for other cases (where usually the duct stumps are small and multiple). The conclusion was that the laparoscopic technology is a good option in view of enhanced vision which facilitates especially the caudate lobectomy.
In the same year, Zhang et al. described a pure laparoscopic right hepatectomy with caudate lobe resection, complete lymph node dissection and hepaticojejunostomy (34). Imaging was consistent with a Bismuth type IIIa hilar cholangiocarcinoma without hepatic artery nor portal vein invasion. Operative time was 590 minutes, blood loss about 300 mL, and hospital stay of 11 days without morbidity. In the author’s opinion the advantage of this procedure is early patient’s recovery and return to chemotherapy.
The largest series of laparoscopic resections for Klatskin tumours associated with hepatectomy have been published during the last 2 years. In 2019, Elmoghazy et al. disclosed the outcomes of 35 patients operated for extrapancreatic biliary cancer (35). Eleven were affected by hilar cholangiocarcinoma and treated with curative intent; lymphadenectomy was performed in 10 patients, and the median number of nodes harvested was 9. In this group, major hepatectomy was performed in 8 and caudate lobectomy in 6 patients, with limited blood loss (250 mL) and transfusion rate (3 patients), and 73% R0 rate. The authors stressed that operative time (355 minutes) and hospital stay (21 days) were higher than in operations performed for gallbladder cancer or intrahepatic cholangiocarcinoma. Similarly the conversion rate (45% vs. 0% and 7%), which reasons were unclear anatomy/resectability or need for revision of the bilioenteric anastomosis. Postoperative morbidity (64%) included 2 liver failure and 4 bile leak, but mostly including minor complications. The 18% mortality rate (one patient for liver failure and one for peritonitis) was at the upper limit if compared to open, however larger, series. The authors commented that Klatskin tumors were the last among extrapancreatic biliary tumours to be approached laparoscopically in their experience in view of the multiple simultaneous skills necessary to complete safe and oncologically adequate resections. Although still in the development phase, their preliminary experience was considered promising. However, they recommended this to be reserved to specialized centres and advocated for further researches.
In the same year, Feng et al. published the results obtained on 9 patients affected by Bismuth type III or IV hilar cholangiocarcinoma and operated by laparoscopy (36). Patients were deemed inadequate for a laparoscopic approach in case of tumoural extension beyond the segmental bile ducts or invasion of the hepatic artery and/or portal vein tributary to the liver remnant. Five left and four right hemiepatectomies with caudate lobectomy were performed, along with extended lymphadenectomy (comprising the celiac trunk, superior mesenteric and para-aortic stations). Bilioenteric anastomosis was performed laparoscopically, whereas the jejunojejunostomy through a 5-cm upper abdominal incision used for the specimen extraction. Operative time was 479 minutes, blood loss 950 mL and transfusion rate 44%. One patient developed bile leak, and one patient died for liver insufficiency: the authors interpreted the long postoperative stay (median 36 days) as strongly influenced by the outcomes of these two patients. However, R0 rate was 100%. Considering the lack of manual palpation during laparoscopy, the authors described carefully their technique for adequate intraoperative staging: dissection of the hilar plate along the wall of the bile duct to expose the bifurcation and secondary ducts; frozen section on margins; extended lymphadenectomy by principle. Through these expedients, the radicality of laparoscopic surgery for Bismuth type III and IV Klatskin tumours was deemed improved.
In addition to the abovementioned, the present literature accounts for two comparative studies in the setting of hilar cholangiocarcinoma. In 2019, Zhang et al. compared 14 laparoscopic and 9 open resections for Bismuth type I–IV Klatskin tumours (37). The authors embarked on these procedures after accumulated experience in laparoscopic pancreatoduodenectomy, caudate lobectomy and other liver resections. The contraindication for laparoscopy was in case vascular resection could not be excluded preoperatively. The distribution of Bismuth type I–IV tumours was not different in the two groups, and hemihepatectomy extended to the caudate lobe was always performed for type III and IV. Lymphadenectomy was also a standard part of the operation, and a totally laparoscopic technique was used for the bilioenteric reconstruction. Two laparoscopic procedures required conversion because of evidence of portal vein invasion. Unfortunately, no details were reported on the laterality and the proportion of left and right hepatectomies, and their specific outcomes.
We recently published the results of our institutional series of laparoscopic resections for perihilar cholangiocarcinoma versus open, based on propensity score matching (38). During the study period (March 2018–June 2019), patients affected by perihilar cholangiocarcinoma were approached by laparoscopy except those presenting with at least one among preset contraindications: Bismuth type IV; requiring left or right trisectionectomy; evidence of arterial encasement; need for vascular resection/reconstruction; metallic biliary stent in place. The majority of patients had Bismuth type III tumours: left hepatectomy was performed in 56% and 53% of laparoscopic and open operations, right hepatectomy in 44% and 48% respectively. The study group accounted for 16 patients which were compared with a matched control group of 32 open resections selected among patients operated during a previous period (2014–March 2018), so as to reduce the bias of variations in the protocols of perioperative management of different eras. Formal lymphadenectomy of stations 8 and 12 and en bloc resection of Segment 1 were systematically performed. Roux-en-Y loop was performed after the completion of the liver resection, whereas the hepaticojejunostomy was fashioned after specimen extraction through a supraumbilical median incision. The feasibility and safety of laparoscopic operations was supported by the absence of intraoperative accidents and a conversion rate similar to that reported for laparoscopic major liver resections: 3 patients were converted to open (18.8%) for the sake of oncological radicality (intraoperative finding of wider longitudinal/radial spread). Moreover, all converted procedures were right hepatectomies, whereas left-sided resections were all completed. Laparoscopic resections resulted significantly longer (360 versus 275 minutes), but associated with lower intraoperative blood loss (380 versus 470 mL) and transfusions (12.5% versus 21.9%). Despite not statistically significant it was also recorded a lower morbidity rate for laparoscopic operations (43.8% versus 50%), and a significantly shorter length of stay was seen (median 10 versus 14, P=0.048). We commented that the limited sample size of the study group probably influenced the statistical power of the results, and the possibility to record a frank reduction of complications. However, to perform the demolition phase of the operation by laparoscopy and then the reconstructive phase via the service incision seems to provide a smoother postoperative course (as often associated with minimally-invasive approaches). We do not exclude that future larger studies may be able to detect a reduction of specific complications such as infectious. Regarding oncologic results, final histology showed a comparable number of harvested lymph nodes between the two groups (median 12 versus 11, P=NS) and R0 rate not statistically different (81% versus 53% respectively). We concluded that the traditional skepticism and conceptual obstacles regarding laparoscopic approach may be overcome in the next future, given the adequate safety and feasibility for selected patients showed by expert centres in this exploratory phase.
Robotic resections
In 2010, Giulianotti et al. from Chicago (USA) described an extended right hepatectomy with hepaticojejunostomy for a hilar cholangiocarcinoma by the use of the da Vinci Robotic Surgical System (Intuitive Surgical, Sunnyvale, CA, USA) (39). Preoperative imaging showed no infiltration of the hilar vessels, and the patient was treated with portal vein embolization. The robotic phase of the operation included the lymphadenectomy of the common hepatic artery. The specimen was retrieved from a 7 cm midline laparotomy, through which a Roux-en-Y anastomosis was performed in order to speed up the procedure, whereas the left hepaticojejunostomy was performed robotically after restarting of the pneumoperitoneum, allowing a bilioenteric anastomosis on a small bile duct. The duration of surgery was 540 minutes and the estimated blood loss of 800 mL with one unit of red blood cells transfused. Postoperative course was uneventful and the patient discharged 11 days after. Final histology confirmed a T2 bile duct adenocarcinoma without lymph node positivity and resection margins free from tumor. This was a first commendable report of the feasibility and safety of robotics applied to major hepatobiliary surgery for hilar cholangiocarcinoma. Among the author’s highlights, the added value of increased degrees of freedom of instruments and 3D magnified vision for facilitating the construction of the biliary anastomosis. It was also underlined that increasing experience could probably reduce the total postoperative stay, which was relatively long in this case. However, it has to be noted that no information were provided on the number of lymph nodes retrieved and that the caudate lobe was not resected.
Although ten years have passed since this report, only a handful of other researches have been published on robotics for these procedures. In 2012, Liu et al. described 64 robotic surgeries for biliary malignancies, with the primary endpoint to investigate the incidence of port-site metastasis (40). Among 39 patients affected by hilar cholangiocarcinoma, 3 of them underwent left hemihepatectomy with bile duct confluence resection and reconstruction. Mortality was nihil. However, the authors did not provide information on the techniques for reconstruction, on regional lymphadenectomy nor caudate lobe resection, nor in the specific morbidity rates in this subgroup.
In 2014, Zhu et al. performed a robotic two-stage surgery for a patient with a Bismuth type IIIa tumour elected to biliary resection and right hemihepatectomy (41). The first procedure consisted in a robotic bile duct exploration, external drainage of the left hepatic duct with a T-tube, hilar dissection of the right hepatic artery and portal branches with placement of a vascular device as a tourniquet for occlusion of the right hepatic pedicle. The patient underwent a second admission for occlusion of the right hepatic vascular inflow to induce the left hemiliver hypertrophy. After three weeks, the patient was treated with a robotic right hemihepatectomy, biliary confluence resection with hepaticoenterostomy. The procedure was successfully performed, with 700 mL blood loss, 2 weeks postoperative stay and R0 resection margin at final histology. The publication lacks of details on the performance of lymphadenectomy, caudate lobe resection, and postoperative morbidity. However, the authors highlighted some advantages of this two-stage technique, including the assessment of diagnosis and tumour margins at the first stage, the possibility to enhance hypertrophy by both right portal and arterial occlusion, and the low invasiveness of robotics as a mean to favour recovery and complementary treatments.
The largest series has been published recently by Li et al. (42). The authors described 48 robotic radical resections for hilar cholangiocarcinoma. The majority of patients was treated for Bismuth type I or IIIb adenocarcinomas, while patients with stage T4 tumours or preoperative chemotherapy/radiotherapy were excluded. Similarly, Bismuth type IV neoplasms were judged inadequate for robotic approach, since trisectionectomy is generally required to achieve radical resection, and given the associated challenges to manage intraoperative bleedings for these kind of resections. Unfortunately, also this series lacks of description of the numerosity of patients treated with liver resection. It can only be extrapolated that caudate lobectomy was the standard, 30-days reoperation and mortality rates were nihil. Regarding oncologic outcomes, it was shown an R1 rate similar to that of previous researches: 9 cases after local excision for type I or II tumours, and 4 cases after left hemihepatectomy for IIIb. The authors concluded that robotic resection can be a valid alternative to open for selected Bismuth type I, II or III cholangiocarcinomas, but called for larger studies with longer follow-up durations to evaluate appropriately the long-term outcomes.
So far, there is only one comparative study with the open technique. In 2016, Xu et al. disclosed the results of 10 robot-assisted liver and bile duct confluence resection for hilar cholangiocarcinoma, compared with 32 laparotomic resections (43). The robotic group included 4 left hemihepatectomies, 5 right hemihepatectomies and 1 right trisectionectomy for Bismuth type II, IIIa/b or IV tumours. All hemihepatectomies were associated with caudate lobectomy, even if the paracaval portion was left in place in some cases due to difficult exposure. Locoregional lymphadenectomy of stations 8, 12 and 13 was routinely performed. Totally robotic Roux-en-Y and bilioenteric anastomoses were performed, except one hybrid approach. No conversion occurred, and no deaths related to technical issues was recorded. The authors concluded that the feasibility of oncologically radical resections for hilar cholangiocarcinoma is technically achievable.
Discussion
In 2019, a systematic review on minimally-invasive surgery for cholangiocarcinoma was published (44). The study meta-analyzed perioperative and oncological outcomes of both robotic and pure laparoscopic operations, including 3-year recurrence free and overall survival. Regarding hilar cholangiocarcinoma, a single study comparing robotic and open techniques was retrieved (43). As such, only a pooled analysis of 9 non-comparative studies was possible. Its results showed that 90% of patients received major hepatectomy, and the estimate size for overall morbidity was 51%. Given the scarcity of publications, no other information could be pooled, including the oncologic data. This documents that the technique is still in its development phase and uptaken with caution worldwide. Moreover, the available evidence is various in selection criteria, outcomes reporting and description of techniques. Many publications lack of details on caudate lobectomy, extent of the lymphadenectomy, number of lymph nodes retrieved and clear exclusion criteria. Despite the available data are promising, laparoscopic surgery for hilar cholangiocarcinoma only benefits of preliminary reports on its feasibility and safety, and is still far from firm information on oncologic adequacy, ideal candidates, standardized technique and possible advantages. With regard to robotics for hilar cholangiocarcinoma, it was interesting to note that it has been reported before pure laparoscopy, contrarily to what has happened for liver resections for intrahepatic malignancies (39). The inherent advantages associated with robotics gives reason of this forward application: enhanced dexterity, refined vision are described as major facilitations for anastomosis, lymphadenectomy and major hepatectomies associated with caudate resection. However, no additional publications of robot-assisted liver resections have been published from the same groups after their initial and limited series. This suggests that this technique as well is still being applied selectively and spreading slowly even in those units that have started their learning curve 10 years far ago. It would be interesting to know whether any of these renowned surgical groups has abandoned the minimally-invasive program for hilar cholangiocarcinomas after its initiation. All the authors concluded advocating for large, and possibly prospective, studies to obtain more robust information on the added value of minimally-invasive approaches for Klatskin tumours. Stratification of results according to the type of surgical operation is expected, in particular for those procedures for which a concomitant liver resection is recommended.
Conclusions
It is advocated further research on this topic to include a larger number of patients, standardize the technique especially for the most difficult steps and refine the reconstructive phase. However, the actual data should not foster theoretical hostility toward the implementation of minimally-invasive techniques in this setting, but rather support its stepwise advancements in expert centres.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Giammauro Berardi) for the series “Minimally Invasive Resections for Liver Malignancies: Among Certainties and Controversies” published in Laparoscopic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/ls-20-95
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls-20-95). The series “Minimally Invasive Resections for Liver Malignancies: Among Certainties and Controversies” was commissioned by the editorial office without any funding or sponsorship. LA serves as an unpaid editorial board member of Laparoscopic Surgery from Oct 2017 to Nov 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hasegawa S, Ikai I, Fujii H, et al. Surgical resection of hilar cholangiocarcinoma: analysis of survival and postoperative complications. World J Surg 2007;31:1256-63. [Crossref] [PubMed]
- DeOliveira ML, Cunningham SC, Cameron JL, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg 2007;245:755-62. [Crossref] [PubMed]
- Yubin L, Chihua F, Zhixiang J, et al. Surgical management and prognostic factors of hilar cholangiocarcinoma: experience with 115 cases in China. Ann Surg Oncol 2008;15:2113-9. [Crossref] [PubMed]
- Sakamoto Y, Kosuge T, Shimada K, et al. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery 2005;137:396-402. [Crossref] [PubMed]
- Nimura Y, Hayakawa N, Kamiya J, et al. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 1990;14:535-43; discussion 544. [Crossref] [PubMed]
- Dinant S, Gerhards MF, Busch OR, et al. The importance of complete excision of the caudate lobe in resection of hilar cholangiocarcinoma. HPB (Oxford) 2005;7:263-7. [Crossref] [PubMed]
- Kondo S, Hirano S, Ambo Y, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg 2004;240:95-101. [Crossref] [PubMed]
- Unno M, Katayose Y, Rikiyama T, et al. Major hepatectomy for perihilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci 2010;17:463-9. [Crossref] [PubMed]
- Neuhaus P, Jonas S, Bechstein WO, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999;230:808-18; discussion 819. [Crossref] [PubMed]
- Rassam F, Roos E, van Lienden KP, et al. Modern work-up and extended resection in perihilar cholangiocarcinoma: the AMC experience. Langenbecks Arch Surg 2018;403:289-307. [Crossref] [PubMed]
- Aldrighetti L, Belli G, Boni L, et al. Italian experience in minimally invasive liver surgery: a national survey. Updates Surg 2015;67:129-40. [Crossref] [PubMed]
- Aldrighetti L, Cipriani F, Fiorentini G, et al. A stepwise learning curve to define the standard for technical improvement in laparoscopic liver resections: complexity-based analysis in 1032 procedures. Updates Surg 2019;71:273-83. [Crossref] [PubMed]
- Cipriani F, Ratti F, Paganelli M, et al. Laparoscopic or open approaches for posterosuperior and anterolateral liver resections? A Propensity Score based analysis of the degree of advantage. HPB (Oxford) 2019;21:1676-86. [Crossref] [PubMed]
- Cipriani F, Fantini C, Ratti F, et al. Laparoscopic liver resections for hepatocellular carcinoma. Can we extend the indication in cirrhotic patients? Surg Endosc 2018;32:617-26. [Crossref] [PubMed]
- Kasai M, Cipriani F, Gayet B, et al. Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient’s data. Surgery 2018;163:985-95. [Crossref] [PubMed]
- Berardi G, Van Cleven S, Fretland ÅA, et al. Evolution of Laparoscopic Liver Surgery from Innovation to Implementation to Mastery: Perioperative and Oncologic Outcomes of 2,238 Patients from 4 European Specialized Centers. J Am Coll Surg 2017;225:639-49. [Crossref] [PubMed]
- Berardi G, Aghayan D, Fretland A, et al. Multicentre analysis of the learning curve for laparoscopic liver resection of the posterosuperior segments. Br J Surg 2019;106:1512-22. [Crossref] [PubMed]
- Puntambekar S, Sharma V, Kumar S, et al. Laparoscopic Management of Hilar Cholangiocarcinoma: a Case Report. Indian J Surg 2016;78:57-9. [Crossref] [PubMed]
- Hu HJ, Wu ZR, Jin YW, et al. Minimally invasive surgery for hilar cholangiocarcinoma: state of art and future perspectives. ANZ J Surg 2019;89:476-80. [Crossref] [PubMed]
- Abu Hilal M, Aldrighetti L, Dagher I, et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann Surg 2018;268:11-8. [Crossref] [PubMed]
- Patriti A, Cipriani F, Ratti F, et al. Robot-assisted versus open liver resection in the right posterior section. JSLS 2014;18:e2014.00040.
- Guan R, Chen Y, Yang K, et al. Clinical efficacy of robot-assisted versus laparoscopic liver resection: a meta analysis. Asian J Surg 2019;42:19-31. [Crossref] [PubMed]
- Ratti F, Fiorentini G, Cipriani F, et al. Perioperative and Long-Term Outcomes of Laparoscopic Versus Open Lymphadenectomy for Biliary Tumors: A Propensity-Score-Based, Case-Matched Analysis. Ann Surg Oncol 2019;26:564-75. [Crossref] [PubMed]
- Fiorentini G, Ratti F, Cipriani F, et al. Challenges and Technical Innovations for an Effective Laparoscopic Lymphadenectomy in Liver Malignancies. J Laparoendosc Adv Surg Tech A 2019;29:72-5. [Crossref] [PubMed]
- Cipriani F, Ratti F, Cardella A, et al. Laparoscopic versus open major hepatectomy: analysis of clinical outcomes and cost-effectiveness in a high-volume centre. J Gastrointest Surg 2019;23:2163-73. [Crossref] [PubMed]
- Cipriani F, Alzoubi M, Fuks D, et al. Pure laparoscopic versus open hemihepatectomy: a critical assessment and realistic expectations. A propensity score-based analysis of right and left hemihepatectomies from 9 European tertiary referral centers. J Hepatobiliary Pancreat Sci 2020;27:3-15. [Crossref] [PubMed]
- Fiorentini G, Ratti F, Cipriani F, et al. Tips and Tricks for a Laparoscopic Approach to Paracaval Liver Segments. Ann Surg Oncol 2018;25:1695-8. [Crossref] [PubMed]
- Yu H, Wu SD, Chen DX, et al. Laparoscopic resection of Bismuth type I and II hilar cholangiocarcinoma: an audit of 14 cases from two institutions. Dig Surg 2011;28:44-9. [Crossref] [PubMed]
- Machado MA, Makdissi FF, Surjan RC, et al. Laparoscopic resection of hilar cholangiocarcinoma. J Laparoendosc Adv Surg Tech A 2012;22:954-6. [Crossref] [PubMed]
- Machado MA, Makdissi FF, Surjan RC. Totally laparoscopic right hepatectomy with Roux-en-Y hepaticojejunostomy for right-sided intraductal papillary mucinous neoplasm of the bile duct. Ann Surg Oncol 2014;21:1841-3. [Crossref] [PubMed]
- Gumbs AA, Jarufe N, Gayet B. Minimally invasive approaches to extrapancreatic cholangiocarcinoma. Surg Endosc 2013;27:406-14. [Crossref] [PubMed]
- Lee W, Han HS, Yoon YS, et al. Laparoscopic resection of hilar cholangiocarcinoma. Ann Surg Treat Res 2015;89:228-32. [Crossref] [PubMed]
- Li J, Zhao L, Zhang J, et al. Application of the laparoscopic technique in perihilar cholangiocarcinoma surgery. Int J Surg 2017;44:104-9. [Crossref] [PubMed]
- Zhang CW, Liu J, Hong DF, et al. Pure laparoscopic radical resection for type IIIa hilar cholangiocarcinoma. Surg Endosc 2018;32:1581-82. [Crossref] [PubMed]
- Elmoghazy W, Cowan J, Tabchouri N, et al. Liver resection for extra-pancreatic biliary cancer: what is the role of laparoscopic approach? Surg Endosc 2019;33:3711-7. [Crossref] [PubMed]
- Feng F, Cao X, Liu X, et al. Laparoscopic resection for Bismuth type III and IV hilar cholangiocarcinoma: How to improve the radicality without direct palpation. J Surg Oncol 2019;120:1379-85. [Crossref] [PubMed]
- Zhang Y, Dou C, Wu W, et al. Total laparoscopic versus open radical resection for hilar cholangiocarcinoma. Surg Endosc 2020;34:4382-7. [Crossref] [PubMed]
- Ratti F, Fiorentini G, Cipriani F, et al. Perihilar cholangiocarcinoma: are we ready to step towards minimally invasiveness? Updates Surg 2020;72:423-33. [Crossref] [PubMed]
- Giulianotti PC, Sbrana F, Bianco FM, et al. Robot-assisted laparoscopic extended right hepatectomy with biliary reconstruction. J Laparoendosc Adv Surg Tech A 2010;20:159-63. [Crossref] [PubMed]
- Liu QD, Chen JZ, Xu XY, et al. Incidence of port-site metastasis after undergoing robotic surgery for biliary malignancies. World J Gastroenterol 2012;18:5695-701. [Crossref] [PubMed]
- Zhu Z, Liu Q, Chen J, et al. Robotic surgery twice performed in the treatment of hilar cholangiocarcinoma with deep jaundice: delayed right hemihepatectomy following the right-hepatic vascular control. Surg Laparosc Endosc Percutan Tech 2014;24:e184-90. [Crossref] [PubMed]
- Li J, Tan X, Zhang X, et al. Robotic radical surgery for hilar cholangiocarcinoma: A single-centre case series. Int J Med Robot 2020;16:e2076 [Crossref] [PubMed]
- Xu Y, Wang H, Ji W, et al. Robotic radical resection for hilar cholangiocarcinoma: perioperative and long-term outcomes of an initial series. Surg Endosc 2016;30:3060-70. [Crossref] [PubMed]
- Shiraiwa DK, Carvalho PFDC, Maeda CT, et al. The role of minimally invasive hepatectomy for hilar and intrahepatic cholangiocarcinoma: A systematic review of the literature. J Surg Oncol 2020;121:863-72. [Crossref] [PubMed]
Cite this article as: Cipriani F, Ratti F, Fiorentini G, Aldrighetti L. Minimally invasive liver resections for hilar cholangiocarcinoma: a narrative review. Laparosc Surg 2021;5:36.


