Regional anaesthetic in a laparoscopic transabdominal preperitoneal inguinal hernia repair
Introduction
Spinal anaesthesia in laparoscopic hernia surgery is a relatively new concept and we present a case report on a male patient who underwent a left inguinal herniorrhaphy through a transabdominal preperitoneal (TAPP) approach. The majority of published studies have documented spinal anaesthesia in the transabdominal extraperitoneal approach (TEPP) which does not involve the peritoneal cavity and has historically been associated with fewer complications (1).
The authors present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/ls-20-96).
Case presentation
Methods
Patient selection and workup
A 44-year-old male presented to our surgical service for investigation of his left groin pain that had been present for a few months. The pain was accompanied by a palpable bulge to the left groin. There was no radiation of the pain, however, it got worse on heavy lifting or physical straining. He gave no recent trauma history. Clinical examination revealed a left indirect inguinal hernia that was reducible. The rest of his abdominal examination was unremarkable.
During a discussion about surgery and possible complications the patient mentioned that he had a spinal anaesthetic for his previous knee surgery and wondered whether this was possible for his hernia surgery.
Pre-operative preparation
The patient was referred to the pre-anaesthesia clinic (PAC) to examine the feasibility of a regional anaesthetic for his laparoscopic herniorrhaphy. At PAC, his anaesthetist deemed him a low surgical risk for a spinal anaesthetic. He consented to a laparoscopic TAPP repair as well as a spinal anaesthetic after the complications of both techniques were discussed.
Equipment preference card
The TAPP under regional anaesthesia required two distinct lists of equipment; one for the anaesthetic procedure and a second for the surgical procedure. Please refer to Table 1 for the full list of equipment used.
Table 1
| Description | |
|---|---|
| Surgeon | Dr. Yagan Pillay |
| Procedure | Left inguinal herniorrhaphy TAPP approach |
| Position | Trendelenburg with left side up |
| Glove size/style | 8.0 |
| Equipment | Standard laparoscopic equipment: camera, monitor, light source |
| A 30° laparoscope | |
| 1× 5-mm trocar and 1× 12-mm disposable trocar and 1× 10-mm trocar | |
| Laparoscopic tacker with absorbable tackers | |
| Laparoscopic suction irrigation device | |
| Supplies | Laparoscopic tray with scalpel/forceps and sens retractors |
| Towel packs: 2 | |
| Sterile gowns and gloves for sterile team members | |
| Suture pack (2-0 vicryl and 4-0 monocryl, 1 pack each) | |
| Instrumentation | Laparoscopic Maryland forceps, hook dissector and bowel probe |
| Laparoscopic Ligasure© device | |
| Anaesthetist | Dr. Victor Asefa |
| Procedure | Spinal anaesthesia |
| Position | Sitting position |
| Glove size/style | 7.5 |
| Equipment | Sterile skin preparation materials (3M SoluPrep©: 2% chlorhexidine gluconate and 70% v/v isopropyl alcohol) |
| Sedatives: Midazolam© 2 mg & Fentanyl© citrate 100 mcg | |
| Local anaesthetic: | |
| Spinal: 0.75% Bupivacaine© HCL in dextrose (2 mL) + 15 mcg Fentanyl© | |
| Epidural top-up: 2% Lidocaine© (5 mL) + 0.25% Bupivacaine© (5 mL) | |
| IV cannula and dressings for cannula (18G left hand vein) | |
| Epidural/spinal needles: | |
| Tuohy© needle; halyard© 17 G ×3.5 | |
| Spinal 25 G ×5 BD Whitacre© needle | |
| Resuscitation equipment: | |
| Phenylephrine 10 mg in 100 mL 0.9% normal saline | |
| Ephedrine 50 mg in 10 mL 0.9% normal saline | |
| Oxygen mask/AMBU bag; 7.5/8.0 ETT | |
| Propofol 10 mg/mL (20 mL) | |
| Rocuronium 10 mg/mL (10 mL) | |
| Supplies | Sterile gowns and gloves for sterile team members |
| Chlorhexidine with alcohol drape | |
| Anaesthetic machine, cylinders, oxygen masks | |
| Emergency/resuscitation drugs | |
| Instrumentation | Respirator and vitals monitors (ECG, BP monitor-3 minutes interval, pulse oximeter) |
Procedure
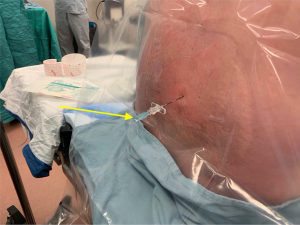
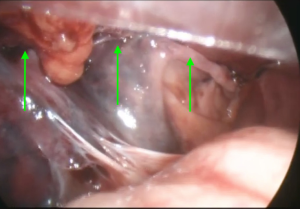
Our patient had a combined spinal epidural (CSE) and aseptic technique was maintained throughout. He was appropriately positioned on the operating table. His lumbar area was prepped using 3M SoluPrep© large swabs. The recommended spinal level of L3/L4 interstate was identified and 1% Lidocaine© infiltrated into skin and fascia. A 17 G Tuohy© needle was inserted and the epidural space identified by loss of resistance to air. A 25 G Whitacre© 5-inch needle was subsequently inserted into the intrathecal space. Clear cerebrospinal fluid (Figure 1) was visualized in the Whitacre© needle and 2 mL of 0.75% Bupivacaine© in dextrose + 15 mcg Fentanyl© was injected into the intrathecal space. The spinal needle was removed and an epidural catheter inserted with a 7 cm skin level. Finally, the Tuohy© needle was withdrawn and the catheter secured in place with Tegaderm© and tape. The patient was then positioned supinely and his anaesthetic level tested and marked at T8 on his abdominal wall prior to surgery (Figure 2). Intravenous sedation of Midazolam© 2 mg, and Fentanyl© 100 mcg was given prior to surgical incision. At insertion of the pneumoperitoneum the patient complained of shoulder pain, and an epidural top-up, consisting of 5 mL 2% Lidocaine© and 5 mL 0.25% Bupivacaine© was given. This created the requisite analgesic control for his shoulder pain.
The surgery itself was uneventful and the left indirect inguinal hernia was laparoscopically repaired using a self-adherent mesh, through a TAPP approach.
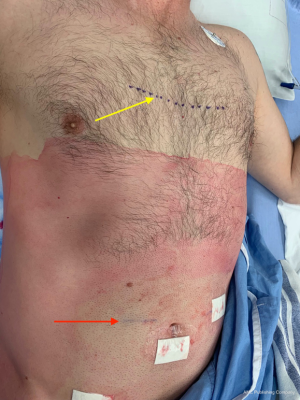
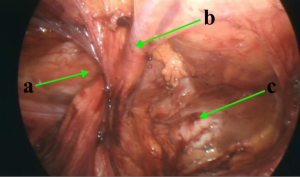
A laparoscopic Ligasure© device was used to open the preperitoneal space until the surgical landmarks were obtained (Figure 3). Self-adherent mesh was inserted (Figure 4) and the mesh was re-peritonealised once its position was confirmed (Figure 5). The patient had adequate pain control intraoperatively and was even able to visualize his laparoscopic herniorrhaphy on the surgery monitor.
Role of team members
Victor Asefa: anaesthetist who performed the regional anaesthetic; Yagan Pillay: surgeon who performed the laparoscopic TAPP herniorrhaphy. There was also a surgical assistant, a scrub nurse, an anaesthesia nurse and a rotating floor nurse.
Results
Post-operative management
His anaesthesia level was marked post-operatively due to the clinical migration of his sensory level cephalad to his nipples (Figure 6). The patient made an uneventful recovery with none of the recognized hernia or spinal anaesthetic complications. This included inguinodynia, headache, hypotension, urinary retention, nausea and vomiting. The spinal anaesthetic was recovered prior to his discharge on the same day.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
Discussion
Spinal anaesthesia in the laparoscopic TAPP repair has not been well documented. There has been one clinical trial to date in the published literature (2). Proponents of the TEPP approach have pointed to the use of regional anaesthetic as one of the advantages of their technique over the TAPP approach (3). This case report helps to substantiate the validity of regional anaesthesia in the TAPP approach and it is our hope to expand this into a case series or a randomized controlled trial.
The patient was extremely happy with his outcome and did not use any analgesia until the second post-operative day. He did not require opiates for analgesic control. This concept of decreased analgesic use for pain control following a spinal anaesthetic is well documented in the literature (4).
Surgical facilitation to accommodate the regional anaesthesia included a pneumoperitoneum of 10 mmHg, use of a self-adherent mesh, and marking of the patient’s anaesthesia level on his abdominal wall so as to document any intraoperative pain issues. Post-operative migration of the anaesthesia level, a common issue with spinal anaesthesia, was also documented (5), due undoubtedly to the patient`s Trendelenburg position during his surgery.
The obvious advantage of this technique lies in the lack of positive pressure ventilation which in the past has been an issue with patients with American Society of Anesthesiologists (ASA) 3 & 4 scores. These patients had open surgery for their hernias due to the high anaesthetic risk associated with their poor respiratory physiology. If laparoscopic TAPP hernia surgery can be performed under spinal anaesthetic these patients will reap the well documented effects of laparoscopic herniorrhaphy over open herniorrhaphy (6).
An unintended advantage of this technique is the voluntary increase in abdominal pressure by getting the patient to cough during surgery. This intraoperative Valsalva maneuver in the peritoneal cavity allows for a pressure effect against the mesh in the preperitoneal space. It allowed us to laparoscopically visualize the mesh in situ covering the hernial neck. This helped ascertain adequate mesh overlap prior to mesh re-peritonealisation. In order to improve future outcomes, our thought is to monitor the mesh with an intraoperative ultrasound in future patients to confirm adequate hernial neck overlap.
Conclusions
We present a case report of a spinal anaesthetic in a laparoscopic inguinal hernia TAPP approach. It is our belief that this technique is as valid as the regional anaesthetic in the TEPP approach and will serve as a template for further studies into regional anaesthetic and laparoscopic TAPP herniorrhaphy. The inguinal hernias of high-risk surgical patients could be laparoscopically managed in an optimal manner with further substantiation of the scientific validity of spinal anaesthesia and the TAPP approach.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/ls-20-96
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls-20-96). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Köckerling F, Bittner R, Jacob DA, et al. TEP versus TAPP: comparison of the perioperative outcome in 17,587 patients with a primary unilateral inguinal hernia. Surg Endosc 2015;29:3750-60. [Crossref] [PubMed]
- Sarakatsianou C, Georgopoulou S, Baloyiannis I, et al. Spinal versus general anesthesia for transabdominal preperitoneal (TAPP) repair of inguinal hernia: Interim analysis of a controlled randomized trial. Am J Surg 2017;214:239-45. [Crossref] [PubMed]
- Sarhan AE, Sherif T, El-Kenany Y. Open preperitoneal mesh repair versus laparoscopic transabdominal preperitoneal repair of groin hernia under spinal anesthesia: results of a prospective randomized multicenter trial. Egypt J Surg 2016;35:132-9. [Crossref]
- Donmez T, Erdem VM, Sunamak O, et al. Laparoscopic total extraperitoneal repair under spinal anesthesia versus general anesthesia: a randomized prospective study. Ther Clin Risk Manag 2016;12:1599-608. [Crossref] [PubMed]
- Lee MH, Kim EM, Bae JH, et al. Head elevation in spinal-epidural anesthesia provides improved hemodynamics and appropriate sensory block height at caesarean section. Yonsei Med J 2015;56:1122-7. [Crossref] [PubMed]
- Yildirim D, Hut A, Uzman S, et al. Spinal anesthesia is safe in laparoscopic total extraperitoneal inguinal hernia repair. A retrospective clinical trial. Wideochir Inne Tech Maloinwazyjne 2017;12:417-27. [Crossref] [PubMed]
Cite this article as: Pillay Y, Asefa R, Asefa V. Regional anaesthetic in a laparoscopic transabdominal preperitoneal inguinal hernia repair. Laparosc Surg 2020;4:46.