
Mesh placement for hiatal hernia repair: can we solve the controversy?
Introduction
Guidelines for the Management of Hiatal Hernia published by the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) (1) describe hiatal hernia as a common disorder characterized by the protrusion of abdominal structures other than esophagus into the thoracic cavity. Anatomic criteria permit categorization into four subtypes. Around 95% of all hiatal hernias are type I. Although only type II is pure paraesophageal hernia (PEH), types III and IV are also referred to as PEH and are becoming increasingly more common with the aging of the population. Over 90% of large hiatal hernias are type III hernias, with a large part of the stomach herniating into the mediastinum (2). The S.A.G.E.S guidelines recommend that patients’ age and comorbidities be considered before routine elective repair of asymptomatic PEH is decided. Nevertheless, patients with truly asymptomatic PEH are rare. Heartburn and reflux are common in less severe stages while post-prandial chest fullness or shortness of breath are frequent in patients with larger hernias (2).
Correct PEH repair involves complete reduction of the mediastinal sac with a wide esophageal mobilization and a tension-free hiatal closure (3). However, a tension-free cruroplasty is not easy, and recurrence has been reported in up to 42% of cases (4). In an effort to lower recurrence rates, Kuster and Gilroy introduced synthetic mesh (SM) reinforcement in 1993 (5) and several studies have since reported a decrease in recurrence rates with its use (6,7). Nevertheless, severe complications have also been reported (8-10) and biological mesh (BM) has been proposed as an alternative. Results regarding the efficacy of mesh, however, are conflicting (11). While long-term clinical results are good, several studies (12-14) have reported a high radiological recurrence rate.
Recurrence of PEH and influencing factors
The immediate clinical outcome of laparoscopic PEH repair is highly satisfactory (15). However, when compared with the open approach the recurrence rate is higher than expected at midterm follow-up (4,15). In 2000, Hashemi et al. (4) reported an objective recurrence rate (determined by videoesophagram) of 42% after laparoscopic repair of PEH compared with 15% after open repair. One decade later, with the introduction of absorbable mesh reinforcement in 84% of patients and Collis gastroplasty in 40% of patients, they reported a reduction in the hernia recurrence rate similar to that seen with the open approach (16). Several authors have analysed the possible factors influencing the hernia recurrence rate after laparoscopic PEH repair. One reason for failure of the hiatal repair is tension in the lateral portions of the diaphragm near the crura after approaching the pillars of a particularly wide hiatus (15). However, the size of the hernia is not the only factor. The structure of the pillars is also an important anatomical element for the genesis of failure (17). The use of mesh may therefore provide better results because it reinforces hernia repair.
Another aspect influencing the failure of hiatal repair is the length of the esophagus. Laparoscopic pneumoperitoneum elevates the diaphragm and can give surgeons the impression of more intra-abdominal esophagus than there really will be once the diaphragm returns to its normal position with deflation of the pneumoperitoneum (16). In addition, it can be complex to precisely determine the gastroesophageal junction in chronic herniation of proximal stomach (16). In 1957, Collis described the technique for lengthening the esophagus. Currently, the most popular adapted technique creates the gastroplasty tube by excising a wedge of the fundus (18).
The role of the short esophagus in hernia recurrence has been evaluated by several authors, such as Morino et al. (19). In a series of 65 patients submitted to elective laparoscopic repair of large hiatal hernia they found 14 patients had primary closure, 37 received a mesh, and 14 underwent a Collis-Nissen gastroplasty. The recurrence rate was 35% in the mesh group, considerably lower than the 77% in the primary closure group. No recurrences were observed in the Collis-Nissen group, even though a case of distal esophagus perforation requiring esophagectomy and posterior esophagocoloplasty was described in this group. The authors recommend intraoperative evaluation once the hernia dissection has been performed because the correct preoperative diagnosis of a short esophagus is extremely difficult. They also recommend an intraoperative endoscopic evaluation of the esophagogastric junction to decide whether or not Collis-Nissen gastroplasty is required (19).
When should a mesh be placed?
The management of paraesophageal hernias continues to spark controversy. In the last decade, at least 24 systematic reviews and meta-analysis on PEH repair have been published but only four randomized clinical trials (RCTs) have compared PEH repair with and without mesh (see Table 1). One of these RCTs is the trial of Frantzides et al. (6), where the authors compared the laparoscopic repair of hiatal hernia >8 cm with and without polytetrafluoroethylene (PTFE) mesh reinforcement. They reported a recurrence rate of 0/36 vs. 8/36 (22%), respectively, at a median follow-up of 2.5 years. The meta-analysis of Antoniou et al. (23), that included RCTs of Frantzides (6), Granderath (20) and Oelschlager (24), also found a lower incidence of recurrence with the use of mesh. These results appeared to provide a high level of evidence for the use of mesh in hiatal hernia repair. Nevertheless, the follow-up of these studies did not allow conclusions to be drawn regarding the long-term effect. In addition, after a follow-up of more than 4 years, the randomized study of Oelschlager (21) observed no differences in recurrence rates between patients receiving primary repair and those receiving mesh reinforcement. However, we must take into account that while Oelschlager (21,24) used BM, Frantzides (6) and Granderath (20) used SM, and no long-term results have yet been published. A fourth randomized study by Watson et al. (22,25) compared the use of absorbable mesh, nonabsorbable mesh, and primary suture in 126 patients. After a follow-up of only 12 months, they observed that overall outcomes after sutured repair and mesh repair were similar. In another study of note, Zaninotto et al. (26) performed a follow up of 64 months, evaluating patients who underwent mesh surgery by endoscopy every 2 years. They observed that all recurrences occurred within the first eight postoperative months.
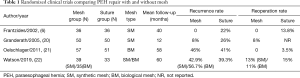
Full table
In a meta-analysis in 2016, Huddy et al. (27) evaluated the results obtained in patients following suture repair (SR), BM or SM repair. They also carried out a survey of surgeons to establish a perspective of current practice. They concluded that both BM and SM reduce the rate of recurrence compared to suture, but they found insufficient evidence regarding the optimum technique if risks and benefits were considered. Other meta-analyses offer similar conclusions regarding the recurrence rate comparing mesh repair vs. suture (see Table 2).
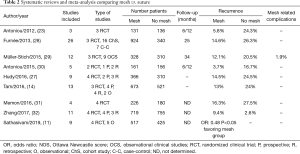
Full table
Due to the lack of convincing RCTs, expert opinion (33,34) was requested to answer questions concerning the use of mesh in PEH repair. Using a Delphi consensus process, Bonrath and Grantcharov (33) attempted to generate information on current practices and highlight key topics of disagreement based on the opinions from a panel of European experts from high-volume centers regarding foregut surgery. Eighteen of the 27 initially identified experts participated throughout the entire consensus process. Consensus was a majority of at least two-thirds of the participants. However, no consensus was reached regarding the importance of mesh use for PEH repair. Only 7 panellists considered the role of mesh reinforcement of the hiatus “important” or “very important”. Nevertheless, the majority (n: 12) felt that mesh use was relevant under specific circumstances. The size of the hiatal defect and the quality of the crura were the factors influencing the decision for mesh use for most individuals who used mesh (10/14). In the same year, Furnée et al. (35) published the results of a web-based questionnaire completed by 165 European upper gastrointestinal (GI) surgeons identified through the European Association for Endoscopic Surgery. The majority of respondents (77.6%, 128 respondents) used mesh selectively, depending on the size of the hiatus, the tension on the sutured cruroplasty, or both.
Which type of mesh should I use?
The characteristics of the mesh used should be taken into consideration. Many different materials and configurations of mesh are available, but consensus regarding the best option is lacking. The Delphi process of Bonrath and Grantcharov (33) did not reach a consensus regarding the type of mesh. Of the 165 surgeons who completed the questionnaire of Furnée et al. (35), 154 reported that they used some type of mesh in hiatal hernia repair (routinely or selectively). The most frequently used types were polypropylene (PP) by 52.6%, followed by expanded PTFE (ePTFE) by 32% and biomesh by 27.9%. The option for the majority was thus an SM. This result is quite different from the results of the survey among SAGES members (36). American surgeons preferred the absorbable type of mesh (67%).
When analyzing the results of RCTs according to the type of mesh favoured, Oelschlager (21) did not observe significantly lower recurrence rates after a long-term follow-up with the use of BM reinforcement. In their review of the literature, Panait et al. (37) reached the conclusion that definitive evidence is still lacking to support the use of biologic or bioabsorbable materials to reinforce hiatal closure in the cure of PEH.
Frantzides (6) and Granderath (20) used SM but their long-term results have not yet been published. Granderath (38), however, published their long-term experience with circular PP mesh reinforcement in a series of 33 patients who underwent laparoscopic refundoplication, and after a follow-up of 60 months, the radiological study revealed a recurrence rate of 6%.
Watson et al.’s randomized study (25) comparing absorbable mesh, nonabsorbable mesh, and primary suture did not identify significant differences in the recurrence rate between groups (23.1% after SR, 30.8% after absorbable mesh, and 12.8% after nonabsorbable mesh). There is no consensus regarding the configuration of the mesh employed (39) but the options seem to have narrowed down somewhat. Furnée et al. (35) stated that at present, the most frequently used configuration is the rectangular or “U” shape, positioned posteriorly to the esophagus.
What about complications with mesh implants?
In 2009, Stadlhuber et al. (40) published a series of 28 patients with mesh-related complications after hiatal hernia repair. Most patients (23 cases) required mesh removal due to intraluminal erosion in 17 cases. Esophagectomy was required in six patients, while another three patients had a partial or total gastrectomy.
For the time being, we cannot establish the exact rate of mesh-associated complications. Müller-Stich et al. (29) analysed their incidence through a systematic review including 124 studies (19 case reports) with a total of 5,499 patients submitted to laparoscopic PEH repair with mesh cruroplasty. They reported 91 (1.9%) mesh-associated complications. The main causes were erosions of the esophagus, the stomach, or the aorta, followed by stenoses and cardiac tamponades. Four fatal complications occurred, all originating from cardiac tamponades due to the staples used for the fixation of the mesh to the hiatus. PP and PTFE were the most frequently used materials (71.5% of patients), followed by BM. Complication rates were 0.8% for PP mesh, 2.5% for PTFE mesh and 1.3% for BM. These results are similar to those observed in two other consecutive patient series where the complication rates published were about 1% (41,42). This incidence may seem low, but the implications are serious. We should take into account that we do not know the real incidence of secondary complications due to migration and erosion because most studies do not include long-term results. However, data available to date seems that around 90% of mesh-related complications occur within two years after surgery (29,39,43).
Müller-Stich et al. (29) described a similar incidence of mesh-related complications for BM and SM, but they did not specify the type of complications due to each type of mesh (BM vs. SM). Serious complications are more commonly associated with synthetic materials and BM is suggested as an alternative. A survey among SAGES members published by Frantzides et al. (44)—and including a total of 5486 PEH repairs—observed that biomaterial tended to be associated with failure while SM tended to be associated with stricture and erosion. PP mesh has the propensity to erode the surrounding tissue over an uncertain period ranging from days to years. It is also known to induce a significant fibrotic reaction, possibly reducing recurrence rates but carrying the risk of complications related to fibrosis of the lower esophagus. PTFE, on the other hand, may lead to high dysphagia rates (33,45). The shape of the mesh must also be considered. Five years ago, the key-hole shape was still used by around 25% of European surgeons (35) compared to 10% of US surgeons according to a report by Frantzides et al. in 2010 (44). The risk of mesh contracting and causing stricture at the gastroesophageal junction is a strong argument against circular positioning (31). Chen et al. (46) initially used a keyhole-shaped mesh, but within 16 months of the operation, three of nine patients required reoperation because the mesh migrated into the oesophagus. They thus switched to a “U”-shaped composite mesh and reported no complications after a follow-up of more than 5 years.
Impact on quality of life (QOL)
Even if the recurrence rate is high, the incidence of patients requiring surgery is low (see Table 3). Zehetner et al. (16) observed that no patients with a recurrent hernia had a serious or catastrophic complication related to the recurrence, suggesting that the natural history of a small recurrent hernia is different from that of the original intrathoracic stomach. Findings from another author support this concept. In their study with a mean follow-up of 11 years, White et al. (51) found 10 hernia recurrences in 31 patients, but only 20% of them were true PEH recurrences and reoperation was necessary only for two patients. Dallemagne (13), with a median follow-up of 118 months, reported a 2% reoperation rate despite an objective recurrence rate of 66%. Their findings are comparable data to those of Targarona et al. (12) who reported a recurrence rate of 46.5% and a reoperation rate of 3.9%.
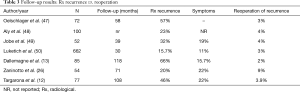
Full table
All authors seem to agree that no surgery is required in cases of recurrence if the patient is asymptomatic. In the European expert consensus published by Bonrath et al. (33) symptomatic recurrence was the only diagnostic factor that achieved agreement for revision surgery. Armijo et al. (52) analyzed a series of 322 patients submitted to PEH repair in order to identify factors that can predict hiatal hernia recurrence. Hernia recurrence was defined as a maximal vertical height of a hernia ≥2 cm above the diaphragm detected by an upper GI contrast study. With a mean follow-up of 20 months, 15.5% of patients had an objective hiatal hernia recurrence, but only 6% of them had a large hiatal hernia (≥5 cm) and required a redo hiatal hernia repair. The overall rate of reoperation was 1%.
Interest also focuses on QOL. In their long-term follow-up series, Targarona et al. (12) reported a mean gastro-intestinal quality of life index (GIQLI) of 111 (range, 59–137) for patients with hiatal recurrence, comparable to that obtained for non-recurrence groups. The results were comparable to those reported by Dallemagne (13). Oelschlager et al. (21,47) analyzed long-term clinical data from the group of patients enrolled in a previously published RCT comparing laparoscopic PEH repair with or without using BM reinforcement. They observed that although radiologic recurrences were frequent, they did not appear to impact on QOL or cause clinical symptoms. They appeared to remain well-controlled, with the exception of hiatal hernias ≥40 mm producing a modest increase in heartburn. Patient satisfaction was high, and the need for reoperation was low. PEH repair with or without BM did not seem to influence QOL. Koetje et al. (53) also analyzed QOL outcomes from their previous published RCT (25), comparing sutures versus repair with BM versus SM. With a follow-up of two years in 72.2% of patients, they observed a significant improvement in QOL, measured by SF-36, with no significant differences between groups.
Conclusions
Since the first data comparing primary suture vs. mesh reinforcement in laparoscopic PEH repair were published around 20 years ago, we continue to ask the same questions: whether to perform hiatoplasty with simple interrupted sutures or with prosthetic material, and if we use a mesh, what material and what shape are the most appropriate.
The heterogeneity of data hinders the interpretation of results. In a systematic review including 26 studies, Furnée et al. (28) observed that only 50% of studies reported the definition of large hiatal herniation and only the 19% of studies used the same definition. The wide variety of materials and shape of the mesh used adds even more heterogeneity.
In conclusion, consensus about the type of mesh continues to be elusive and we clearly need a higher level of evidence to address the controversy. In the meantime, it seems that mesh reinforcement can effectively reduce the hernia recurrence rate. Mesh-associated complications are few, but because they are serious most experts recommend mesh use only in specific circumstances, particularly those in relation to the size of the hiatal defect and the quality of the crura.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Andrea Balla) for the series “Minimally Invasive Approach for the Treatment of Gastro-esophageal Reflux Disease” published in Laparoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls-20-89). The series “Minimally Invasive Approach for the Treatment of Gastro-esophageal Reflux Disease” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kohn GP, Price RR, Demeester SR, et al. Guidelines for the Management of Hiatal Hernia. Society of American Gastrointestinal and Endoscopic Surgeons, 2013. Available online: https://www.sages.org/publications/guidelines/guidelines-for-the-management-of-hiatal-hernia/
- Dallemagne B, Quero G, Lapergola A, et al. Treatment of giant paraesophageal hernia: pro laparoscopic approach. Hernia 2018;22:909-19. [Crossref] [PubMed]
- Nason KS, Luketich JD, Witteman BP, et al. The laparoscopic approach to paraesophageal hernia repair. J Gastrointest Surg 2012;16:417-26. [Crossref] [PubMed]
- Hashemi M, Peters JH, DeMeester TR, et al. Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 2000;190:553-60; discussion 560-1. [Crossref] [PubMed]
- Kuster GG, Gilroy S. Laparoscopic technique for repair of paraesophageal hiatal hernias. J Laparoendosc Surg 1993;3:331-8. [Crossref] [PubMed]
- Frantzides CT, Madan AK, Carlson MA, et al. A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs simple cruroplasty for large hiatal hernia. Arch Surg 2002;137:649-52. [Crossref] [PubMed]
- Carlson MA, Richards CG, Frantzides CT. Laparoscopic prosthetic reinforcement of hiatal herniorrhaphy. Dig Surg 1999;16:407-10. [Crossref] [PubMed]
- Nandipati K, Bye M, Yamamoto SR, et al. Reoperative intervention in patients with mesh at the hiatus is associated with high incidence of esophageal resection-a single-center experience. J Gastrointest Surg 2013;17:2039-44. [Crossref] [PubMed]
- Tatum RP, Shalhub S, Oelschlager BK, et al. Complications of PTFE mesh at the diaphragmatic hiatus. J Gastrointest Surg 2008;12:953-7. [Crossref] [PubMed]
- Parker M, Bowers SP, Bray JM, et al. Hiatal mesh is associated with major resection at revisional operation. Surg Endosc 2010;24:3095-101. [Crossref] [PubMed]
- Sathasivam R, Bussa G, Viswanath Y, et al. Mesh hiatal hernioplasty vs suture cruroplasty in laparoscopic para-oesoophageal hernia surgery; a systematic review and meta-analysis. Asian J Surg 2019;42:53-60. [Crossref] [PubMed]
- Targarona EM, Grisales S, Uyanik O, et al. Long-term outcome and Quality of life after laparoscopic treatment of large paraesophageal hernia. World J Surg 2013;37:1878-82. [Crossref] [PubMed]
- Dallemagne B, Kohnen L, Perretta S, et al. Laparoscopic repair of paraesophageal hernia. Long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann Surg 2011;253:291-6. [Crossref] [PubMed]
- Tam V, Winger DG, Nason KS. A systematic review and meta-analysis of mesh vs suture cruroplasty in laparoscopic large hiatal hernia repair. Am J Surg 2016;211:226-38. [Crossref] [PubMed]
- Targarona EM, Bendahan G, Balagué C, et al. Mesh in the Hiatus. A Controversial Issue. Arch Surg 2004;139:1286-96. [Crossref] [PubMed]
- Zehetner J, DeMeester SR, Ayazi S, et al. Laparoscopic versus Open Repair of Paraesophageal hernia: The Second Decade. J Am Coll Surg 2011;212:813-20. [Crossref] [PubMed]
- Granderath FA, Carlson MA, Champion JK, et al. Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 2006;20:367-79. [Crossref] [PubMed]
- Johnson AB, Oddsdottir M, Hunter JG. Laparoscopic Collis gastroplasty and Nissen fundoplication. A new technique for the management of esophageal foreshortening. Surg Endosc 1998;12:1055-60. [Crossref] [PubMed]
- Morino M, Giaccone C, Pellegrino L, et al. Laparoscopic management of giant hiatal hernia: factors influencing long-term outcome. Surg Endosc 2006;20:1011-6. [Crossref] [PubMed]
- Granderath FA, Schweiger UM, Kamolz T, et al. Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg 2005;140:40-8. [Crossref] [PubMed]
- Oelschlager BK, Pellegrini CA, Hunter J, et al. Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 2011;213:461-8. [Crossref] [PubMed]
- Watson DI, Thompson SK, Devitt PG, et al. Five Year Follow-up of a Randomized Controlled Trial of Laparoscopic Repair of Very Large Hiatus Hernia With Sutures Versus Absorbable Versus Nonabsorbable Mesh. Ann Surg 2020;272:241-7. [Crossref] [PubMed]
- Antoniou SA, Antoniou GA, Koch OO, et al. Lower Recurrence Rates After Mesh-reinforcer Versus Simple Hiatal Hernia Repair: A Meta-analysis of Randomized Trials. Surg Laparosc Endosc Percutan Tech 2012;22:498-502. [Crossref] [PubMed]
- Oelschlager BK, Pellegrini CA, Hunter J, et al. Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 2006;244:481-90. [PubMed]
- Watson DI, Thompson SK, Devitt PG, et al. Laparoscopic repair of very large hiatus hernia with sutures vs absorbable vs non-absorbable mesh-a randomized controlled trial. Ann Surg 2015;261:282-9. [Crossref] [PubMed]
- Zaninotto G, Portale G, Constantini M, et al. Objective follow-up after laparoscopic repair of large type III hiatal hernia. Assessment of safety and durability. World J Surg 2007;31:2177-83. [Crossref] [PubMed]
- Huddy JR, Markar SR, Ni MZ, et al. Laparoscopic repair of hiatus hernia: Does mesh type influence outcome? A meta-analysis and European survey study. Surg Endosc 2016;30:5209-21. [Crossref] [PubMed]
- Furnée E, Hazebroek E. Mesh in laparoscopic large hiatal hernia repair: a systematic review of the literature. Surg Endosc 2013;27:3998-4008. [Crossref] [PubMed]
- Müller-Stich BP, Kenngott HG, Gondan M, et al. Use of Mesh in Laparoscopic Paraesophageal Hernia Repair: A Meta-Analysis and Risk-Benefit Analysis. PLoS One 2015;10:e0139547. [Crossref] [PubMed]
- Antoniou SA, Müller-Stich BP, Antoniou GA, et al. Laparoscopic augmentation of the diaphragmatic hiatus with biologic mesh versus suture repair: a systematic review and meta-analysis. Langenbecks Arch Surg 2015;400:577-83. [Crossref] [PubMed]
- Memon MA, Memon B, Yurus RM, et al. Suture Cruroplasty Versus Prosthetic Hiatal Herniorrhaphy for Large Hiatal Hernia: A Meta-analysis and Systematic Review of Randomized Controlled Trials. Ann Surg 2016;263:258-66. [Crossref] [PubMed]
- Zhang C, Liu D, Li F, et al. Systematic review and meta-analysis of laparoscopic mesh versus suture repair of hiatus hernia: objective and subjective outcomes. Surg Endosc 2017;31:4913-22. [Crossref] [PubMed]
- Bonrath EM, Grantcharov TP. Contemporary management of paraesophaegeal hernias: establishing a European expert consensus. Surg Endosc 2015;29:2180-95. [Crossref] [PubMed]
- Graham B, Regehr G, Wright JG. Delphi as a method to establish consensus for diagnostic criteria. J Clin Epidemiol 2003;56:1150-6. [Crossref] [PubMed]
- Furnée EJB, Smith CD, Hazebroek EJ. The use of mesh in laparoscopic large hiatal hernia repair: a survey of European Surgeons. Surg Laparosc Endosc Percutan Tech 2015;25:307-11. [Crossref] [PubMed]
- Pfluke JM, Parker M, Bowers SP, et al. Use of mesh for hiatal hernia repair: a survey of SAGES members. Surg Endosc 2012;26:1843-48. [Crossref] [PubMed]
- Panait L, Novitsky YW. Hiatal Hernia Repair: Current Evidence for Use of Absorbable Mesh to Reinforce Hiatal Closure. Surg Technol Int 2017;30:182-7. [PubMed]
- Granderath FA, Granderath UM, Pointner R. Laparoscopic revisional fundoplication with circular hiatal mesh prosthesis: the long-term results. World J Surg 2008;32:999-1007. [Crossref] [PubMed]
- Granderath FA. Measurement of the esophageal hiatus by calculation of the hiatal surface area (HSA). Why, when and how? Surg Endosc 2007;21:2224-5. [Crossref] [PubMed]
- Stadlhuber RJ, Sherif AE, Mittal SK, et al. Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 2009;23:1219-26. [Crossref] [PubMed]
- Dally E, Falk GL. Teflon pledget reinforced fundoplication causes symptomatic gastric and esophageal lumenal penetration. Am J Surg 2004;187:226-9. [Crossref] [PubMed]
- Müller-Stich BP, Koninger J, Muller-Stich BH, et al. Laparoscopic mesh-augmented hiatoplasty as a method to treat gastroesophageal reflux without fundoplication: single-center experience with 306 consecutive patients. Am J Surg 2009;198:17-24. [Crossref] [PubMed]
- De Moor V, Zalcman M, Delhaye M, et al. Complications of mesh repair in hiatal surgery: about 3 cases and review of the literature. Surg Laparosc Endosc Percutan Tech 2012;22:e222-5. [Crossref] [PubMed]
- Frantzides CT, Carlson MA, Loizides S, et al. Hiatal hernia repair with mesh: a survey of SAGES members. Surg Endosc 2010;24:1017-24. [Crossref] [PubMed]
- Antoniou SA, Koch OO, Antoniou GA, et al. Mesh-reinforced hiatal hernia repair: a review on the effect on postoperative dysphagia and recurrence. Langenbecks Arch Surg 2012;397:19-27. [Crossref] [PubMed]
- Chen Z, Zhao H, Sun X, et al. Laparoscopic repair of large hiatal hernias: clinical outcomes of 10 years. ANZ J Surg 2018;88:E703-7. [Crossref] [PubMed]
- Oelschlager BK, Petersen RP, Brunt LM, et al. Laparoscopic paraesophageal hernia repair: Defining Long-Term Clinical and Anatomic Outcomes. J Gastrointest Surg 2012;16:453-9. [Crossref] [PubMed]
- Aly A, Munt J, Jamieson GG, et al. Laparoscopic repair of large hiatal hernias. Br J Surg 2005;92:648-53. [Crossref] [PubMed]
- Jobe BA, Aye RW, Deveney CW, et al. Laparoscopic management of giant type III hiatal hernia and short esophagus. Objective follow-up at three years. J Gastrointest Surg 2002;6:181-8. [Crossref] [PubMed]
- Luketich JD, Nason KS, Christie NA, et al. Outcomes after a decade of laparoscopic giant paraesophageal hernia repair. J Thorac Cardiovasc Surg 2010;139:395-404. [Crossref] [PubMed]
- White BC, Jeansonne LO, Morgenthal CB, et al. Do recurrences after paraesophageal hernia repair matter? Ten-year follow-up after laparoscopic repair. Surg Endosc 2008;22:1107-11. [Crossref] [PubMed]
- Armijo PR, Pokala B, Misfeldt M, et al. Predictors of Hiatal Hernia Recurrence after Laparoscopic Anti-reflux Surgery with hiatal hernia repair: a Prospective Database Analysis. J Gastrointest Surg 2019;23:696-701. [Crossref] [PubMed]
- Koetje JH, Irvine T, Thompson SK, et al. Quality of Life following repair of Large Hiatal Hernia is Improved but not influenced by use of mesh: Results from a Randomized Controlled Trial. World J Surg 2015;39:1465-73. [Crossref] [PubMed]
Cite this article as: Balagué C, Fdez-Ananín S, Sacoto D, Targarona EM. Mesh placement for hiatal hernia repair: can we solve the controversy? Laparosc Surg 2021;5:6.


