Laparoscopic pancreaticojejunal anastomosis using knotless barbed absorbable sutures are simple, safe and effective: an experience with 34 procedures
Introduction
Since the first description of a laparoscopic pancreas resection by Gagner et al. (1) in 1994 minimally invasive pancreaticoduodenectomy has drawn a lot of attention. Most of the studies show that in the hands of experienced laparoscopic surgeons the procedure is technically feasible and just as safe as open pancreaticoduodenectomy but longer follow-up intervals and larger series are probably required to assess whether they have similar oncologic outcomes (2-4) and the increased use of robotic surgery augments the feasibility of complete minimally invasive pancreaticoduodenectomy (5).
Over time most of the important issues addressing the actual resection step of the procedure have been addressed, with most of the authors agreeing that an artery first approach is recommended and is one of the advantages of the laparoscopic approach (6,7). We have previously described our artery-first approach to pancreaticoduodenectomy (6) and the aim of the current article is to focus on the pancreaticojejunostomy technique.
An extensive review of the literature shows that current studies focus on two aspects that might be causes for pancreatic fistulas—the type of anastomosis used (duct-to-mucosa or invaginating anastomosis) (8-10) and the texture of pancreas (5,11,12). In our case the reconstruction is performed using a barbed suture end-to-side pancreaticojejunostomy and the aim of our study was to verify the effectiveness of this type of anastomosis.
Methods
Description of the technique
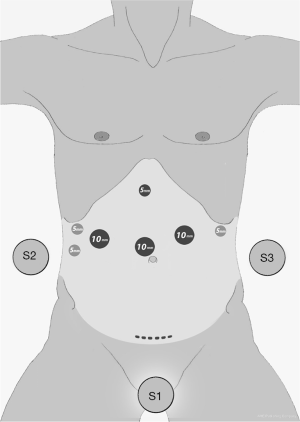
The patient is positioned in a semi-Fowler’s position with legs apart. Under general anesthesia, using a Veress needle (Ethicon Endo-Surgery Inc., Cincinnati, OH) inserted in the left hypochondriac region the pneumoperitoneum is induced at a pressure of 14 mm Hg and the trocars are inserted under direct vision. The surgeon is placed between the patient’s legs, with an assistant on each side, as shown in Figure 1. The trocar positioning used by our team has been previously described in our previous article describing our artery-first approach (6).
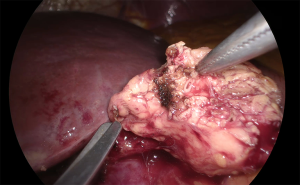
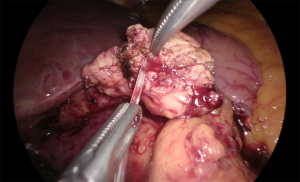
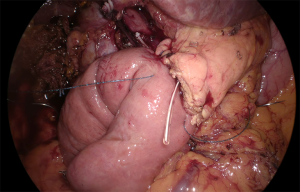
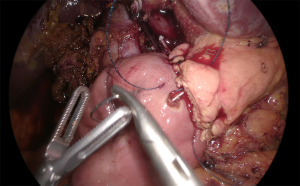
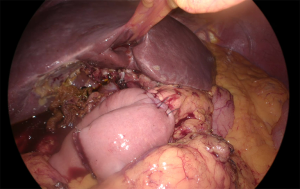
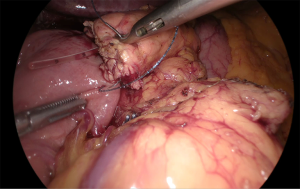
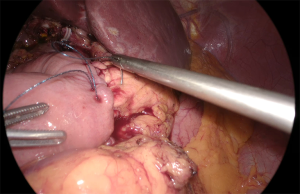
The pancreaticojejunostomy is performed in an end-to-side manner (Video 1). The Wirsung duct is catheterized before the anastomosis using an adapted silicone drain, depending on the size of the duct (Figures 2,3). The anastomosis is done by performing a posterior and an anterior full-thickness running suture with a resorbable, barbed, self-locking 3/0 V-Loc ® suture (Covidien, USA), as shown in Figures 3-8.
At the end of the reconstruction the greater omentum is positioned posterior to the pancreaticojejunostomy in order to isolate the anastomosis from the mesenteric vessels. We prefer to systematically use 2 Penrose drains, one guarding the pancreaticojejunostomy, which exits the abdomen through the left lateral-most 10 mm trocar and one guarding the hepaticojejunal anastomosis, exiting through the right lateral-most 5 mm trocar.
For the purpose of the study we analyzed a retrospective series of 34 consecutive cases of laparoscopic pancreaticoduodenectomies operated between January 2016 and April 2019. The written informed consent was obtained from the patients for publication of this study and any accompanying images.
Results
In total, a number of 19 (55.88%) women and 15 (44.12%) men were enrolled in the study.
We recorded a 9 (26.47%) leak rate with 6 (17.65%) type A fistulas and 3 (8.82%) type B fistulas. No type C fistulas and no deaths were recorded due to postoperative complications.
There were 25 (73.53%) soft pancreases and 9 (26.47%) firm pancreases. The size of the Wirsung duct was 1 mm in 4 (11.76%) of the patients, 2 mm in 6 (17.65%) of the patients, 3–4 mm in 19 (55.88%) of the patients and above 4 mm in 5 (14.71%) of the cases. There were no conversions to other types of anastomoses, no biliary fistulas or stenoses, no hemorrhagic complications and only one conversion to laparotomy. The time required to perform the anastomosis was 17.3±6.7 minutes (range, 10.6–24 minutes).
From a point of view of the pathology results we found:
- 24 (70.59%) pancreatic ductal adenocarcinomas;
- 4 (11.76%) distal cholangiocarcinomas;
- 2 (5.88%) pseudotumoral chronic pancreatitis;
- 1 (2.94%) ampuloma;
- 1 (2.94%) cystic dystrophy of the duodenal wall;
- 1 (2.94%) duodenal adenocarcinoma;
- 1 (2.94%) duodenal sarcoma.
Discussion
Laparoscopic pancreaticoduodenectomy has been a reason for debate ever since the first article describing it in 1994, when even authors conclude that despite it being feasible from a technical view, unlike other minimally invasive procedures it might not bring a major benefit in terms of morbidity and mortality (1). Nowadays, more and more studies agree on the fact that compared with open pancreaticoduodenectomy, the minimally invasive procedure has similar complication rates (2,4,13) whilst bringing advantages such as better assessment of resectability through a posterior artery-first approach (6,14) and an optimized intraoperative assessment of anatomic aberrations (7,14). A separate question whose answer would require larger randomized control trials is the question of the oncologic quality of resection (2-4). From our point of view such randomized control trials are difficult to be performed because groups performing open pancreaticoduodenectomy are convinced of the superiority of it and vice versa for the groups performing the same procedure minimally invasive.
The purpose of this paper is to present the technique we use for our pancreaticojejunostomies. Two out of the three anastomoses required for the reconstruction of the continuity of the digestive tract after pancreaticoduodenectomy—the pancreaticojejunostomy and the gastro-jejunostomy are based on the use of barbed, self-locking sutures. Out of these two anastomoses the pancreaticojejunostomy is the most complication prone and has raised most of the debates in literature (8-10). The reasons why we prefer using such sutures are as follows: our previous experience in using them for other digestive tract anastomoses (15,16), our experience in laparoscopic pancreaticoduodenectomy (4,6) and an extensive review of the literature showing that our type of anastomosis using barbed sutures is feasible and safe for patients regardless of the texture of the pancreatic stump (9-12).
The concern that pancreatic fistulas might arise as a complication depending on the type of pancreaticojejunostomies has been approached by Kennedy et al. (10) in a study comparing the two most spread techniques for pancreaticojejunostomy, the duct-to-mucosa anastomosis and the invaginating or “dunking” pancreaticojejunostomy. Besides their own experience Kennedy et al. quote two large randomized control trials comparing these anastomotic techniques, the Berger trial and the Bassi trial because of the significant differences between the results of the two studies. In the first trial Bassi et al. (8) report on a group of 144 patients that they found no significant difference between the rate of complications of the two types of anastomosis while in the study published by Berger et al. (9) significantly fewer pancreatic fistulas are reported when using the invaginating pancreaticojejunostomy.
A secondary outcome of the Berger trial shows a higher rate of pancreatic fistulas in the case of patients with softer glands compared to harder glands (9). Regarding the consistency of the pancreatic stump another study by Battal et al., assessing the difficulties encountered when switching from open to laparoscopic pancreaticoduodenectomy, come to a somewhat counterintuitive conclusion that because of the consistency of the gland, older fit patients are more appropriate for total laparoscopic reconstruction than younger patients (5). As you can very well see from the data presented above, most of the pancreases in our study were soft 73.53% (25/34) and despite that we recorded a 26.47% (9/34) leak rate with 17.65% (6/34) type A fistulas and 8.82% (3/34) type B fistulas an no (0) type C fistulas. The overall number of fistulas we had is completely comparable with the leak rates found in a meta-analysis by Lyu et al. comparing duct-to-mucosa anastomosis to the invagination anastomosis, showing that there is no difference between them in terms of postoperative fistulas and other clinically relevant complications (17). One very important aspect in our case is the fact that we had 0 type C fistulas and no mortality.
We consider that protection of the vessels by the interposition of the greater omentum between them and the pancreaticojejunostomy and the systematic drainage of the abdomen using two Penrose drains are extremely important in case complications arise, despite the lack of evidence-based data on these two subjects.
Conclusions
In our experience minimally invasive pancreaticojejunostomy using barbed self-locking sutures is feasible and safe for the patient in the hands of experienced laparoscopic surgeons (laparoscopic hepato-bilio-pancreatic surgeons).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Edoardo Rosso) for the series “Mini-invasive pancreaticoduodenectomy: are we moving from a “feasible” intervention to be considered the standard?” published in Laparoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2020.03.07). The series “Mini-invasive pancreaticoduodenectomy: are we moving from a “feasible” intervention to be considered the standard?” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee. The written informed consent was obtained from the patients for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 1994;8:408-10. [Crossref] [PubMed]
- Gumbs AA, Rodriguez Rivera AM, Milone L, et al. Laparoscopic pancreatoduodenectomy: a review of 285 published cases. Ann Surg Oncol 2011;18:1335-41. [Crossref] [PubMed]
- Fan Y, Zhao Y, Pang L, et al. Successful Experience of Laparoscopic Pancreaticoduodenectomy and Digestive Tract Reconstruction With Minimized Complications Rate by 14 Case Reports. Medicine 2016;95:e3167 [PubMed]
- Mabrut JY, Fernandez-Cruz L, Azagra JS, et al. Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery 2005;137:597-605. [Crossref] [PubMed]
- Battal M, Yilmaz A, Ozturk G, et al. The difficulties encountered in conversion from classic pancreaticoduodenectomy to total laparoscopic pancreaticoduodenectomy. J Minim Access Surg 2016;12:338-41. [Crossref] [PubMed]
- Azagra JS, Arru L, Estevez S, et al. Pure laparoscopic pancreatoduodenectomy with initial approach to the superior mesenteric artery. Wideochir Inne Tech Maloinwazyjne 2015;10:450-57. [Crossref] [PubMed]
- Lupaşcu C, Moldovanu R, Andronic D, et al. Posterior approach pancreaticoduodenectomy: best option for hepatic artery anatomical variants. Hepato-gastroenterology 2011;58:2112-14. [PubMed]
- Bassi C, Falconi M, Molinari E, et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery 2003;134:766-71. [Crossref] [PubMed]
- Berger AC, Howard TJ, Kennedy EP, et al. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, prospective, dual-institution trial. J Am Coll Surg 2009;208:738-47. [Crossref] [PubMed]
- Kennedy EP, Yeo CJ. Dunking pancreaticojejunostomy versus duct-to-mucosa anastomosis. J Hepatobiliary Pancreat Sci 2011;18:769-74. [Crossref] [PubMed]
- Kim EY, Hong TH. Laparoscopic Longitudinal Pancreaticojejunostomy Using Barbed Sutures: an Efficient and Secure Solution for Pancreatic Duct Obstructions in Patients with Chronic Pancreatitis. J Gastrointest Surg 2016;20:861-66. [Crossref] [PubMed]
- Malya FU, Karatepe O, Bektasoglu H, et al. A reliable pancreaticojejunal anastomosis with V-Loc 180 wound closure device for soft pancreatic stump. Hepato-gastroenterology 2014;61:484-88. [PubMed]
- Zhang YH, Zhang CW, Hu ZM, et al. Pancreatic cancer: Open or minimally invasive surgery? World J Gastroenterol 2016;22:7301-10. [Crossref] [PubMed]
- Vallance AE, Young AL, Pandanaboyana S, et al. Posterior Superior Mesenteric Artery First Dissection Versus Classical Approach in Pancreaticoduodenectomy: Outcomes of a Case-Matched Study. Pancreas 2017;46:276-81. [Crossref] [PubMed]
- De Blasi V, Facy O, Goergen M, et al. Barbed versus usual suture for closure of the gastrojejunal anastomosis in laparoscopic gastric bypass: a comparative trial. Obes surg 2013;23:60-3. [Crossref] [PubMed]
- Facy O, De Blasi V, Goergen M, et al. Laparoscopic gastrointestinal anastomoses using knotless barbed sutures are safe and reproducible: a single-center experience with 201 patients. Surg endosc 2013;27:3841-45. [Crossref] [PubMed]
- Lyu Y, Li T, Wang B, et al. Selection of pancreaticojejunostomy technique after pancreaticoduodenectomy: duct-to-mucosa anastomosis is not better than invagination anastomosis: A meta-analysis. Medicine 2018;97:e12621 [Crossref] [PubMed]
Cite this article as: Azagra JS, Makkai-Popa ST, Pascotto B, Arru L, De Blasi V, Ramia JM, Ibanez-Aguirre FJ, Goergen M. Laparoscopic pancreaticojejunal anastomosis using knotless barbed absorbable sutures are simple, safe and effective: an experience with 34 procedures. Laparosc Surg 2020;4:27.