Laparoscopic common bile duct exploration
There is ongoing debate regarding the optimal management of choledocholithiasis, which occurs in 10–20% of patients with cholelithiasis. Up to 3–10% of patients undergoing cholecystectomy will have concurrent choledocholithiasis (1). Choledocholithiasis may be diagnosed preoperatively, intraoperatively or postoperatively in patients undergoing cholecystectomy. Diagnostic tests include liver function tests (LFTs), liver ultrasound, CT scan, magnetic resonance cholangiopancreatography (MRCP), and intraoperative cholangiogram (IOC). Diagnosis of choledocholithiasis is not necessarily straightforward, as patients may present with a variety of clinical scenarios ranging from elevated LFTs to dilated intrahepatic ducts and/or common bile duct on imaging to frank choledocholithiasis seen on imaging. However, lab data may be normal in patients with choledocholithiasis (leading to unexpected positive IOC if the latter is performed routinely intraoperatively); alternatively preoperatively choledocholithiasis diagnosed preoperatively may resolve spontaneously in many patients (prior to intervention). We do find MRCP helpful for preoperative planning (especially in the presence of large common bile duct stones).
Historically, before the widespread adoption of laparoscopic surgery, choledocholithiasis was managed primarily with open cholecystectomy and common bile duct exploration (CBDE). The introduction of laparoscopic cholecystectomy (LC), combined with the increasing availability of endoscopic retrograde cholangiopancreatography (ERCP), ushered in the treatment algorithm of ERCP first (in patients with preoperative diagnosis of choledocholithiasis) followed by LC, usually during the same hospital admission. The downside of this clinical practice is that the patient requires two episodes of anesthesia and additional stay in the hospital. Furthermore, although ERCP is highly effective in clearing the common bile duct, there are disadvantages to ERCP including potentially “negative” ERCP (i.e., choledocholithiasis resolved prior to the procedure), and procedural complications including pancreatitis, bleeding and perforation.
An alternative treatment algorithm that has been increasing in popularity in select centers, particularly those with advanced laparoscopic surgeons, involves laparoscopic common bile duct exploration (LCBDE) at the time of LC, depending on the IOC findings. Refinements in surgical techniques combined with improvements in available equipment (e.g., choledochoscopes, stone extraction baskets, etc.) have allowed surgeons to effectively treat choledocholithiasis in a single-stage, laparoscopic procedure. Single stage LCBDE has been shown to be highly effective and safe with a low complication rate (2). A recent meta-analysis demonstrated that LCBDE and LC is superior to ERCP followed by LC in terms of perioperative safety and long-term postoperative efficacy (3).
Indications
LCBDE is indicated when choledocholithiasis has been diagnosed preoperatively and the requisite surgeon skill set and equipment are available. LCBDE is also indicated in patients with altered anatomy (e.g., patients post Roux-en-Y gastric bypass) where traditional ERCP may be difficult or impossible. Contraindications include patients with severe hemodynamic instability; however, a potential exception to this may include a patient with severe cholangitis where ERCP or percutaneous transhepatic cholangiography is not available and choledochotomy (with drainage of the duct and placement of T-tube) may be required.
Surgeon requirements
Surgeons who perform LCBDE should have (4):
- A thorough knowledge of biliary anatomy;
- The ability to perform and interpret an IOC;
- An understanding of the different approaches to the common bile duct and tailor the approach to the clinical situation;
- The ability to utilize different techniques of stone extraction (flushing, balloon extraction, basket extraction, choledochoscopy);
- The ability to perform intracorporeal suturing when a choledochotomy is performed.
Equipment
The following equipment is needed for LCBDE:
- C-arm for IOC;
- Cholangiogram catheter to perform IOC;
- Our preference is the 4.5-Fr Taut (Teleflex medical; Wayne PA) cholangiogram catheter passed through a 14-gauge angiocath in the right upper quadrant;
- Alternatively, a 4 or 5 Fr ureteral catheter can be used;
- Glucagon 1 mg intravenous (given by the anesthesiologist to relax the sphincter of Oddi);
- Flexible video choledochoscope;
- Our preference is the 8.5-Fr choledochoscopes (Karl Storz Endoscopy-America; El Segundo, CA) with 3.6-Fr (1.2 mm) inner diameter working channel with picture-in-picture capability of the primary laparoscopic monitor.
- IV tubing for saline instillation through the choledochoscope;
- Pressurized IV-bag set-up;
- Atraumatic graspers to minimize damage to the choledochoscope;
- Fogarty balloon catheters (sizes 4–6 Fr);
- Stone retrieval baskets (Boston Scientific, Natick, MA, USA) including;
- Zero tip nitinol retrieval basket (1.9 to 2.4 Fr);
- Seguira basket (2.4 Fr).
- T-tube (12 Fr, 14 Fr) if indicated;
- 4-0 PDS sutures (RB-1 needle) or equivalent;
- Electrohydraulic or laser lithotripter to fragment impacted stones.
Other resources
- It is also important to have a nursing team familiar with the above equipment to help troubleshoot as indicated;
- If feasible, it may help to have a second circulating nurse for the biliary endoscopy portion of the case.
Technique
Patient positioning is similar to LC. The patient is supine with one arm tucked (depending on the location of the C-arm). Hasson trocar is placed supraumbilical, a 10-mm epigastric trocar is placed (for the 10-mm right angle dissector and clip applier), and two 5-mm ports are placed on the right side, one at the level of the umbilicus at the anterior axillary line, and one just superior to the umbilicus at the mid-clavicular line.
The dome of the gallbladder is retracted cephalad to expose the cystic triangle. The peritoneum of the triangle is incised, the critical structures are exposed, and then a ductotomy is made in the cystic duct. The cholangiocatheter is introduced via a 14-gauge angiocath placed in the right upper quadrant, flushed, and then inserted into the cystic duct and clipped in place. The purpose of flushing the catheter prior to inserting it into the cystic duct is to minimize air bubbles misread as choledocholithiasis on the IOC.
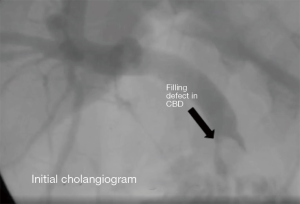
If the IOC reveals some small choledocholithiasis, the next step is to ask the anesthesiologist to give 1 mg glucagon IV, wait 2 minutes and then repeat the cholangiogram. If there are still filling defects noted, then the next step is usually transcystic CBDE. The surgeon can use the IOC to determine the likelihood of success with transcystic CBDE vs. requiring choledochotomy. For instance, small stones are likely to be successfully cleared with transcystic CBDE; however large stones may require choledochotomy, especially if the cystic duct is not dilated (Figure 1).
An additional 5-mm trocar is placed in the subcostal area in the mid-clavicular line. While the nursing staff is setting up the choledochoscope, a 4- or 5-Fr Fogarty is inserted through this additional trocar, into the cystic duct and into the duodenum. If there is difficulty inserting the catheter into the common bile duct due to a tortuous cystic duct, then it may helpful to dissect the cystic duct closer to the common bile duct junction and then creating a new ductotomy. The balloon is inflated and then retracted back into the cystic duct. Cholangiogram may be repeated to see if the duct has been cleared; if the IOC reveals persistent filling defects, then the next step is transcystic choledochoscopy.
The 7-Fr choledochoscope is inserted through the subcostal trocar and into the common bile duct and ideally into the duodenum first. Then with the saline running, biliary endoscopy is performed to identify choledocholithiasis. Any visualized stones can be extracted utilizing a stone extraction basket placed through the working channel of the choledochoscope.
If stones are visualized but unable to be extracted, then the surgeon has the choice of completing the cholecystectomy and obtaining an ERCP postoperatively vs. performing a choledochotomy. If the common bile duct is normal-sized (non-dilated) or if the difficulty in the transcystic CBDE is due to low insertion of the cystic duct, our preference is to defer choledochotomy and obtain postoperative ERCP which, in our experience, has been 100% successful in clearing the duct. In these situations, the surgeon should consider leaving a JP drain at the cystic duct stump in case a leak develops postoperatively (the patient may be at higher chance in the context of ongoing biliary obstruction).
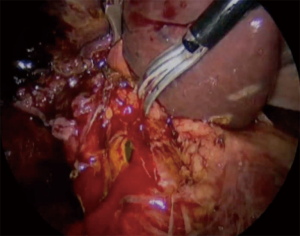
However, if there are large (>1 cm) stones, or if ERCP was attempted preoperatively but unsuccessful, then our preference is to proceed with choledochotomy. An additional 5-mm trocar is placed in the left subcostal area to facilitate suturing. The peritoneum overlying the common bile duct is incised and the anterior surface of the common bile duct is completely exposed. Two 4-0 PDS stay sutures are placed at the medial and lateral aspect of the common bile duct, usually near the cystic duct insertion. A longitudinal choledochotomy is performed sharply with endoshears (Figure 2). It is important to perform the choledochotomy longitudinally and not transversely to preserve the blood supply to the common bile duct.
The 5- or 6-Fr Fogarty catheter is inserted to extract the stones. In our experience, Fogarty catheter is very effective in clearing most stones via choledochotomy. The choledochoscope is reinserted to confirm clearance of the duct. If an impacted stone is seen and unable to be extracted options include laser lithotripsy or, in rare cases, transduodenal sphincteroplasty. Alternatively, a t-tube can be placed with the plan for postoperative ERCP/lithotripsy.
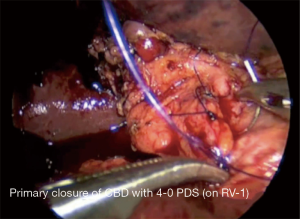
Once the duct has been cleared, then the surgeon must decide whether to place a t-tube. Primary closure (without t-tube) is acceptable, especially if the surgeon is confident that the duct has been cleared (5,6). T tube drainage has been shown to result in significantly increased operative time and may be associated with complications such as biliary leakage. However, if there is any concern regarding the caliber of the common bile duct (or narrowing during closure) or retained stones, then the surgeon should consider placing a t-tube. The closure of the common bile duct is usually performed with 4-0 PDS sutures on RB-1 needle (our preference is interrupted simple sutures; Figure 3). Our preference is to leave a JP drain at the choledochotomy site.
Discussion
Laparoscopic CBDE is a safe and effective technique in addressing common bile duct stones. Combined with cholecystectomy, it allows for single stage management for patients with choledocholithiasis. Transcystic CBDE in particular is a safe procedure that can be taught to surgeons and housestaff. In the majority of cases, if transcystic CBDE is not successful, postoperative ERCP is effective in clearing the duct.
Evidence from several studies demonstrate that single stage LC and LCBDE is superior to ERCP and then LC for the management. One of the barriers to this treatment algorithm is the perceived barriers to learning the technical aspects of LCBDE. Nationally chief residents graduate on average with one CBDE based on Surgery Accreditation Council for Graduate Medical Education case logs. We have made a concerted effort at our institution to teach the surgical housestaff the basics of transcystic CBDE, reserving choledochotomy for select circumstances. In our experience, >90% of choledocholithiasis can be managed effectively with transcystic CBDE, deferring choledochotomy for select cases. Over the past several years, our graduating chief residents now graduate with 3.2 CBDE/year (94%ile) while the national average has remained relatively unchanged.
Conclusions
LCBDE is a safe and effective technique for management of choledocholithiasis. Transcystic CBDE can be learned by housestaff and can be used to manage most patients with choledocholithiasis, reserving postoperative ERCP for unsuccessful transcystic CBDE and deferring choledochotomy for select situations (large stones, altered anatomy, etc.)
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Laparoscopic Surgery for the series “Laparoscopic Surgery of the Liver and Spleen”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2019.12.06). The series “Laparoscopic Surgery of the Liver and Spleen” was commissioned by the editorial office without any funding or sponsorship. HLP serves as the unpaid Guest Editor of this series and serves as an unpaid editorial board member of Laparoscopic Surgery from Feb 2019 to Jan 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol 2006;12:3162-7. [Crossref] [PubMed]
- Di Mauro D, Ricciardi E, Siragusa L, Manzelli A. Outcome of Laparoscopic Common Bile Duct Exploration After Failed Endoscopic Retrograde Cholangiopancreatography: A Comparative Study. J Laparoendosc Adv Surg Tech A 2019;29:1391-6. [Crossref] [PubMed]
- Pan L, Chen M, Ji L, et al. The Safety and Efficacy of Laparoscopic Common Bile Duct Exploration Combined with Cholecystectomy for the Management of Cholecysto-choledocholithiasis: An Up-to-date Meta-analysis. Ann Surg 2018;268:247-53. [Crossref] [PubMed]
- Zerey M, Haggerty S, Richardson W, et al. Laparoscopic common bile duct exploration. Surg Endosc 2018;32:2603-12. [Crossref] [PubMed]
- Martin I, Bailey I, Rhodes M, et al. Towards t-tube free laparosocpic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg 1998;228:29-34. [Crossref] [PubMed]
- Gurusamy KS, Koti R, Davidson BR. T-tube drainage versus primary closure after laparoscopic common bile duct exploration. Cochrane Database Syst Rev 2013;CD005641 [PubMed]
Cite this article as: Kelly T, Parikh M, Pachter HL. Laparoscopic common bile duct exploration. Laparosc Surg 2020;4:16.