
Laparoscopic liver resection for large hepatocellular carcinoma
In the journal Surgical Endoscopy, Levi Sandri and Spoletini et al. reported a two-center experience with the short- and long-term outcomes of laparoscopic liver resection (LLR) for large hepatocellular carcinoma (HCC) (1). A total of 172 patients from two high-volume liver surgery centers who underwent LLR between 2003 and 2016 were analyzed after classification into three groups according to tumor size (<3 cm, between 3 and 5 cm, and ≥5 cm). Compared with the other groups, the large HCC group (≥5 cm, n=38) had higher conversion rates (18.4%), more frequent and prolonged pedicle clamping, longer operative times [225 (range, 159–270) min], higher blood loss [300 (range, 75–800) mL], and longer total hospital [6 (range, 4–8) d] and intensive care unit stays [1 (range, 0–1) d]. No differences in morbidity, mortality, completeness of resection rates, and long-term outcomes were found between the three groups. The authors raised the matter of determining LLR in terms of tumor size and concluded that tumor size does not negatively affect outcomes.
LLR has yielded improved short-term outcomes, specifically shorter hospital stays, decreased blood loss and transfusion, and wider resection margins (2). The long-term survival rate following LLR is also non-inferior to that following open liver resection (2-4). Concerning patient selection for LLR, the international consensus conferences in Louisville [2008] and Morioka [2014] have shown that “minor” LLR can be undertaken as part of standard practice (5,6), whereas major LLR still represents an innovative procedure with incompletely defined risks. However, patient selection criteria in terms of tumor size were not clearly mentioned or suggested. Recently, increasing numbers of hepatobiliary surgeons have adopted laparoscopic techniques in major liver resection, focusing on assessment of the value of LLR. The Southampton Consensus Guidelines [2017] for laparoscopic liver surgery note that major LLR is associated with reduced hospital stays and blood loss, without affecting morbidity, mortality, or completeness of resection (7). These guidelines also refer to limited cohort studies indicating that laparoscopic resection can be employed in large (5–10 cm) and giant (>10 cm) tumors without increasing morbidity or mortality (8,9). Therefore, the study by Levi Sandri and Spoletini et al. raised the following question: “does tumor size matter?”
Comparative studies in English on large liver tumors are scarce. Hwang et al. (10) performed a large retrospective analysis from a single high-volume center, and the analysis included 2,558 solitary HCCs of <10 cm. They demonstrated that non-anatomical resection, microvascular invasion, and tumor size of >5 cm were independent risk factors for both recurrence and overall survival in multivariate analysis and that long-term survival correlated negatively with tumor size and microvascular invasion. They also suggested the inclusion of tumor size for staging. Ettorre et al. (11) compared short-term outcomes of large (5–10 cm) and giant (>10 cm) HCCs and found longer operative times and greater blood loss in the giant HCC group, without increased complications or mortality. In a comparative study of laparoscopic versus open liver resection for large tumors (5–10 cm), the LLR group achieved shorter postoperative hospital stays and lower complication rates with comparable 1- and 3-year overall and disease-free survival rates (8). Shelat et al. compared LLR for large (≥5 cm) versus giant (≥10 cm) malignant tumors and found that the giant tumor group had greater blood loss and longer operative time, without significantly different complication rates (9).
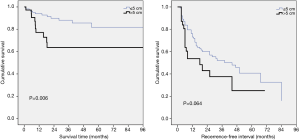
According to the database of our institution, 153 patients underwent LLR for HCCs between 2010 and 2017, comprising 116 with tumor size of ≤5 cm and 37 with tumor size of >5 cm. The large HCC group had more advanced tumor stages (45.9% vs. 5.2% in stage III; P<0.001), higher major liver resection rates (51.4% vs. 12.9%; P<0.001), and higher difficulty scores (8.24 vs. 5.85; P<0.001) than did the small HCC group (12). The large tumor group also had significantly higher blood loss (623.2±841.8 vs. 280.2±439.5 mL; P=0.022), longer operative time (232.5±91.2 vs. 156.8±74.3 min; P<0.001), higher complication rates (18.9% vs. 6.9%; P=0.032), and longer postoperative hospital stays (9.0±5.1 vs. 6.8±4.0 d; P=0.007). No significant difference in recurrence-free survival was found between the two groups (P=0.064), whereas overall survival was significantly higher in the small HCC group (P=0.006) (Figure 1). Long-term outcomes at our institution show similar results to those of the current study. However, all such retrospective studies have the common major shortcoming of evidence because of bias in patient selection.
We follow up with a question about what benefit patients gain in such large tumors. Although no differences in morbidity and mortality were found in terms of tumor size, blood loss and operative time increased in the large tumor group. According to our earlier research, the benefit of LLR appears to decrease slightly with advancing tumor stage; that is, patients in advanced HCC stages obtain fewer benefits from LLR than do those in earlier stages. Although no size cutoff criteria exist for HCC in the current AJCC TNM staging system, large tumors account for a relatively high proportion of advanced-stage HCCs. Therefore, only a limited benefit would be gained if the large tumor group underwent LLR. Moreover, the surgical technique in LLR is highly demanding, and an experienced surgical team including anesthesiologists and intensive care personnel is vital for patient outcomes.
This report by Levi Sandri and Spoletini et al. provides evidence of the short- and long-term outcomes of LLR in relation to tumor size. Other comparative studies as well as our own experience have demonstrated similar results. We suggest that large tumor size (>5 cm) not be viewed as a contraindication of laparoscopic liver surgery by an experienced surgical team and that patient selection is still essential to achieving satisfactory surgical outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Laparoscopic Surgery. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2018.11.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Levi Sandri GB, Spoletini G, Vennarecci G, et al. Laparoscopic liver resection for large HCC: short- and long-term outcomes in relation to tumor size. Surg Endosc 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Jiang B, Yan XF, Zhang JH. Meta-analysis of laparoscopic versus open liver resection for hepatocellular carcinoma. Hepatol Res 2018;48:635-63. [Crossref] [PubMed]
- Aldrighetti L, Guzzetti E, Pulitanò C, et al. Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol 2010;102:82-6. [Crossref] [PubMed]
- Liu K, Chen Y, Wu X, et al. Laparoscopic liver re-resection is feasible for patients with posthepatectomy hepatocellular carcinoma recurrence: a propensity score matching study. Surg Endosc 2017;31:4790-8. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Abu Hilal M, Aldrighetti L, Dagher I, et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann Surg 2018;268:11-8. [Crossref] [PubMed]
- Ai JH, Li JW, Chen J, et al. Feasibility and safety of laparoscopic liver resection for hepatocellular carcinoma with a tumor size of 5-10 cm. PLoS One 2013;8:e72328 [Crossref] [PubMed]
- Shelat VG, Cipriani F, Basseres T, et al. Pure laparoscopic liver resection for large malignant tumors: does size matter? Ann Surg Oncol 2015;22:1288-93. [Crossref] [PubMed]
- Hwang S, Lee YJ, Kim KH, et al. The Impact of Tumor Size on Long-Term Survival Outcomes After Resection of Solitary Hepatocellular Carcinoma: Single-Institution Experience with 2558 Patients. J Gastrointest Surg 2015;19:1281-90. [Crossref] [PubMed]
- Ettorre GM, Levi Sandri GB, Colasanti M, et al. Liver resection for hepatocellular carcinoma ≥5 cm. Transl Gastroenterol Hepatol 2017;2:22. [Crossref] [PubMed]
- Tanaka S, Kubo S, Kanazawa A, et al. Validation of a Difficulty Scoring System for Laparoscopic Liver Resection: A Multicenter Analysis by the Endoscopic Liver Surgery Study Group in Japan. J Am Coll Surg 2017;225:249-258.e1. [Crossref] [PubMed]
Cite this article as: Tsai KY, Huang MT. Laparoscopic liver resection for large hepatocellular carcinoma. Laparosc Surg 2018;2:62.


