The one hundred most-cited articles on laparoscopic liver surgery
Introduction
Since the first laparoscopic liver resection (LLR) was reported in 1992 by Gagner et al. (1) at the Scientific Session of the Society of American Gastrointestinal Surgeons, minimally invasive techniques in liver surgery have continued to develop. LLR is worldwide accepted based on the excellent results shown over the years. The number of publications on LLR increase each year and so the citation index. LLR is certainly one of the fields with the greatest expansion in the scientific surgical community. Despite the fast-growing amount of data, it took 16 years before the first international position on laparoscopic liver surgery was released: The Louisville Statement in 2008 (2).
The present study identifies the 100 most-cited articles related to LLR, analyzes the trends in these articles according to publication year and summarizes on the knowledge and evidence these one-hundred articles brought to the surgical community.
Methods
We performed a search to identify all studies dealing with LLR by utilizing the Institute for Scientific Information (ISI) Web of Science (Thomson Reuters, New York, NY, USA) database. The search was performed on 15 November 2016. We searched the following terms either singly or in combination (“Laparoscopy” liver) OR TITLE: (“Laparoscopic” liver) OR TITLE: (“minimally” liver) OR TOPIC: (“Laparoscopy” hcc) OR TOPIC: (“Laparoscopy” hepatocellular carcinoma) OR TOPIC: (“Laparoscopy” hepatectomy) OR TOPIC: (“Laparoscopy” left lateral) OR TOPIC: (“Laparoscopy” posterior segment); Timespan: All years. Indexes: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI.
Inclusion and exclusion criteria
All article types were potentially included (original articles, review articles, case reports and series, systematic reviews/meta-analyses, letters or commentaries). A LLR article was defined by the following inclusion criteria: (I) content about liver surgery; (II) proposing new technique; (III) comparative study; (IV) indications, classifications and guidelines articles. Exclusion criteria were: (I) study on staging by laparoscopy; (II) non-surgical resection study (i.e., ablation or radiofrequency); (III) robotic surgery.
Results
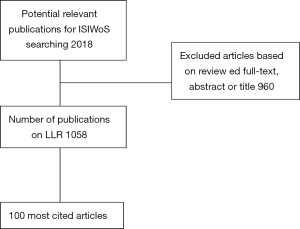
We found 2,018 papers, applying the exclusion criteria on all articles, the 100 most cited articles on LLR were identified (Figure 1). The top 100 articles and their associated number of citations are shown in Table 1. The number of top 100 articles citations ranged from 34 to 364 with a median of 70 (IQR 49–120) citations.
Table 1
| N | Article (authors. title. journal) | Country | Citations |
|---|---|---|---|
| 1 | Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. |
USA | 364 |
| 2 | Buell JF, Cherqui D, Geller DA, |
USA | 352 |
| 3 | Cherqui D, Husson E, Hammoud R, |
France | 313 |
| 4 | Koffron AJ, Auffenberg G, Kung R, |
USA | 260 |
| 5 | Gigot JF, Glineur D, Santiago Azagra J, |
Belgium | 242 |
| 6 | Vibert E, Perniceni T, Levard H, |
France | 213 |
| 7 | Lesurtel M, Cherqui D, Laurent A, |
France | 201 |
| 8 | Kaneko H, Takagi S, Otsuka Y, |
Japan | 181 |
| 9 | Cherqui D, Laurent A, Tayar C, |
France | 180 |
| 10 | Laurent A, Cherqui D, Lesurtel M, |
France | 180 |
| 11 | Buell JF, Thomas MT, Rudich S, |
USA | 179 |
| 12 | Kaneko H, Takagi S, Shiba T. Laparoscopic partial hepatectomy and left lateral segmentectomy: technique and results of a clinical series. |
Japan | 169 |
| 13 | Azagra JS, Goergen M, Gilbart E, |
Belgium | 166 |
| 14 | Morino M, Morra I, Rosso E, |
Italy | 163 |
| 15 | Dagher I, O’Rourke N, Geller DA, |
France | 150 |
| 16 | Descottes B, Glineur D, Lachachi F, |
Belgium | 147 |
| 17 | O’Rourke N, Fielding G. Laparoscopic right hepatectomy: Surgical technique. |
Australia | 141 |
| 18 | Katkhouda N, Hurwitz M, Gugenheim J, |
USA | 130 |
| 19 | Belli G, Fantini C, D’Agostino A, |
Italy | 129 |
| 20 | Dagher I, Proske JM, Carloni A, |
France | 126 |
| 21 | Fong Y, Jarnagin W, Conlon KC, |
USA | 126 |
| 22 | Chang S, Laurent A, Tayar C, |
France | 124 |
| 23 | Cherqui D, Soubrane O, Husson E, |
France | 124 |
| 24 | Castaing D, Vibert E, Ricca L, |
France | 123 |
| 25 | Nguyen KT, Laurent A, Dagher I, |
USA | 121 |
| 26 | Mala T, Edwin B, Gladhaug I, |
Norway | 121 |
| 27 | Rau HG, Buttler E, Meyer G, |
Germany | 121 |
| 28 | Shimada M, Hashizume M, Maehara S, |
Japan | 110 |
| 29 | Viganò L, Laurent A, Tayar C, |
France | 108 |
| 30 | Gayet B, Cavaliere D, Vibert E, |
France | 107 |
| 31 | Descottes B, Lachachi F, Sodji M, |
France | 103 |
| 32 | Bryant R, Laurent A, Tayar C, |
France | 102 |
| 33 | Cho JY, Han HS, Yoon YS, |
Korea | 101 |
| 34 | Tranchart H, Di Giuro G, Lainas P, |
France | 98 |
| 35 | Sasaki A, Nitta H, Otsuka K, |
Japan | 94 |
| 36 | Dagher I, Di Giuro G, Dubrez J, |
France | 93 |
| 37 | Topal B, Fieuws S, Aerts R, |
Belgium | 92 |
| 38 | Gagner M, Rogula T, Selzer D. Laparoscopic liver resection: benefits and controversies. |
USA | 89 |
| 39 | Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. |
Taiwan | 88 |
| 40 | Koffron A, Geller D, Gamblin TC, |
USA | 87 |
| 41 | Soubrane O, Cherqui D, Scatton O, |
France | 85 |
| 42 | Polignano FM, Quyn AJ, de Figueiredo RS, |
UK | 84 |
| 43 | Ishizawa T, Gumbs AA, Kokudo N, |
France | 83 |
| 44 | Yagci G, Ustunsoz B, Kaymakcioglu N, |
Turkey | 82 |
| 45 | Takagi S. Hepatic and portal vein blood flow during carbon dioxide pneumoperitoneum for laparoscopic hepatectomy. |
Japan | 82 |
| 46 | Wakabayashi G, Cherqui D, Geller DA, |
Japan | 81 |
| 47 | Cherqui D. Laparoscopic liver resection. |
France | 80 |
| 48 | Viganò L, Tayar C, Laurent A, |
France | 78 |
| 49 | Dagher I, Belli G, Fantini C, |
France | 74 |
| 50 | Cai XJ, Yang J, Yu H, |
China | 70 |
| 51 | Dulucq JL, Wintringer P, Stabilini C, |
France | 70 |
| 52 | Lin NC, Nitta H, Wakabayashi G. Laparoscopic major hepatectomy: a systematic literature review and comparison of 3 techniques. |
Japan | 67 |
| 53 | Samama G, Chiche L, Bréfort JL, |
France | 67 |
| 54 | Nitta H, Sasaki A, Fujita T, |
Japan | 65 |
| 55 | Feuerstein M, Mussack T, Heining SM, |
Japan | 64 |
| 56 | Gigot JF, Legrand M, Hubens G, |
Belgium | 64 |
| 57 | Burpee SE, Kurian M, Murakame Y, |
USA | 62 |
| 58 | Vanounou T, Steel JL, Nguyen KT, |
Canada | 61 |
| 59 | Cho JY, Han HS, Yoon YS, |
Korea | 61 |
| 60 | Abdel-Atty MY, Farges O, Jagot P |
France | 60 |
| 61 | Lai EC, Tang CN, Ha JP, |
China | 59 |
| 62 | Ito K, Ito H, Are C, |
USA | 58 |
| 63 | Tsinberg M, Tellioglu G, Simpfendorfer CH, |
USA | 58 |
| 64 | Mala T, Edwin B, Rosseland AR, |
Norway | 58 |
| 65 | Dagher I, Lainas P, Carloni A, |
France | 57 |
| 66 | Baker TB, Jay CL, Ladner DP, |
USA | 55 |
| 67 | Yoon YS, Han HS, Cho JY, |
Korea | 54 |
| 68 | Laurent A, Tayar C, Andréoletti M, |
France | 54 |
| 69 | Buell JF, Koffron AJ, Thomas MJ, |
USA | 54 |
| 70 | Khoury G, Abiad F, Geagea T, |
Lebanon | 53 |
| 71 | Diez J, Decoud J, Gutierrez L, |
Argentina | 53 |
| 72 | Abu Hilal M, Underwood T, Zuccaro M, |
UK | 51 |
| 73 | Berber E, Akyildiz HY, Aucejo F, |
USA | 50 |
| 74 | Manterola C, Fernández O, Muñoz S, |
Chile | 50 |
| 75 | Patriti A, Ceccarelli G, Bartoli A, |
Italy | 49 |
| 76 | Cho JY, Han HS, Yoon YS, |
Korea | 49 |
| 77 | Sağlam A. Laparoscopic treatment of liver hydatid cysts. |
Turkey | 49 |
| 78 | Aldrighetti L, Guzzetti E, Pulitanò C, |
Italy | 46 |
| 79 | Koffron AJ, Kung RD, Auffenberg GB, |
USA | 46 |
| 80 | Kazaryan AM, Marangos IP, Røsok BI, |
Norway | 45 |
| 81 | Troisi R, Montalti R, Smeets P, |
Belgium | 45 |
| 82 | Fiamingo P, Tedeschi U, Veroux M, |
Italy | 45 |
| 83 | Kazaryan AM, Pavlik Marangos I, Rosseland AR, |
Norway | 44 |
| 84 | Zhou YM, Shao WY, Zhao YF, |
China | 42 |
| 85 | Ardito F, Tayar C, Laurent A, |
France | 41 |
| 86 | Bickel A, Daud G, Urbach D, |
Israel | 41 |
| 87 | Khoury G, Jabbour-Khoury S, Bikhazi K. Results of laparoscopic treatment of hydatid cysts of the liver. |
Lebanon | 41 |
| 88 | Truant S, Bouras AF, Hebbar M, |
France | 39 |
| 89 | Hüscher CG, Lirici MM, Chiodini S, |
Italy | 39 |
| 90 | Gugenheim J, Mazza D, Katkhouda N, |
France | 39 |
| 91 | Xiong JJ, Altaf K, Javed MA, |
China | 38 |
| 92 | Abu Hilal M, Di Fabio F, Abu Salameh M, |
UK | 38 |
| 93 | Reddy SK, Tsung A, Geller DA. Laparoscopic liver resection. |
USA | 38 |
| 94 | Stoot JH, van Dam RM, Busch OR, |
Netherlands | 38 |
| 95 | Han HS, Cho JY, Yoon YS. Techniques for performing laparoscopic liver resection in various hepatic locations. |
Korea | 36 |
| 96 | Belli G, Fantini C, D’Agostino A, |
Italy | 36 |
| 97 | Tzanis D, Shivathirthan N, Laurent A, |
France | 35 |
| 98 | Cannon RM, Brock GN, Marvin MR, |
USA | 35 |
| 99 | Robles R, Marín C, Abellán B, |
Spain | 34 |
| 100 | Abu Hilal M, Pearce NW. Laparoscopic left lateral liver sectionectomy: a safe, efficient, reproducible technique. |
UK | 34 |
The oldest article was published in 1996 (ranked 12, 13, 56, 77, 88 and 91th) and the most recent in 2015 (45th). Sixty-one articles were published before the first consensus conference held in Louisville in 2008 (published in 2009). Eighty articles were published between 1990 and 2009. The 100 articles were published in 23 different journals (Table 2), 55 articles were published in 3 journals: Surgical Endoscopy [27], Annals of Surgery [20] and British Journal of Surgery [8].
Table 2
| Rank |
|
Number of articles |
|---|---|---|
| 1 |
|
27 |
| 2 |
|
20 |
| 3 |
|
8 |
| 4 |
|
7 |
| 4 |
|
7 |
| 6 |
|
4 |
| 6 |
|
4 |
| 8 |
|
3 |
| 8 |
|
3 |
| 10 |
|
2 |
| 10 |
|
2 |
| 12 |
|
2 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
| 12 |
|
1 |
The most frequent first and last authors were Dagher I (5 articles) and Cherqui D (7 articles) respectively. This result is reflected on the origin of the 100 articles: in 30 cases the article was published by a French team and in 18 cases by a USA team. This means that these two countries have contributed to half of the 100 most important articles on LLR. These results are resumed in Table 3. The topics of the articles were very heterogeneous in 46 cases (e.g., review, feasibility, consensus, personal experience). Nevertheless, if we look at the remaining 54 articles the main topic was: hepatocellular carcinoma in 17 cases, liver cysts of any kind in 9, major hepatectomies in 8, left lateral resections in 7, colorectal metastases in 6, Bening diseases in 4 and in living donor hepatectomies in 3.
Table 3
| Country/author | Number of articles |
|---|---|
| Country | |
| France | 30 |
| USA | 18 |
| Japan | 9 |
| Italy | 7 |
| Belgium | 6 |
| Korea | 5 |
| China | 4 |
| Norway | 4 |
| UK | 4 |
| Lebanon | 2 |
| Turkey | 2 |
| Argentina | 1 |
| Australia | 1 |
| Canada | 1 |
| Chile | 1 |
| Germany | 1 |
| Israel | 1 |
| Netherlands | 1 |
| Spain | 1 |
| Taiwan | 1 |
| First author | |
| Dagher I | 5 |
| Cherqui D | 4 |
| Abu Hilal M | 3 |
| Buell JF | 3 |
| Cho JY | 3 |
| Koffron AJ | 3 |
| Belli G | 2 |
| Descottes B | 2 |
| Gigot JF | 2 |
| Kaneko H | 2 |
| Kazaryan AM | 2 |
| Khoury G | 2 |
| Laurent A | 2 |
| Mala T | 2 |
| Nguyen KT | 2 |
| Viganò L | 2 |
| Last author | |
| Cherqui D | 7 |
| Abecassis M | 4 |
| Fagniez PL | 4 |
| Franco D | 3 |
| Gayet B | 3 |
| Pearce N | 3 |
| Shin SH | 3 |
| Wakabayashi G | 3 |
| Buell J | 2 |
| Dagher I | 2 |
| David A | 2 |
| Edwin B | 2 |
| Gamblin TC | 2 |
| Mathisen O | 2 |
| Shiba T | 2 |
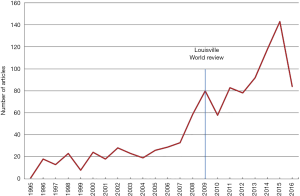
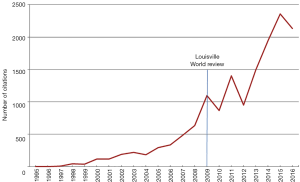
Analyzing the 1,086 articles included in this study, the number of publication grew constantly, with more than 100 publications per year since 2014. The number of citations increased accordingly and it is now of over 2,000 per year (Figures 2,3).
Discussion
Laparoscopic liver surgery is out of doubt one of the fastest growing fields in abdominal surgery today. The technical evolution led to the expansion of the indications without jeopardizing the outcomes. The world review of LLR published in 2009 reported a global experience of 2,804 cases (3). That review is actually the most cited article on LLR. The second most cited article is the first International Position on Laparoscopic Liver Surgery (2).
After the release of the Louisville Statement and the first world review, there has been a substantial increase in the number of published articles and citations per year (namely, >80 articles and >1,000 citations) (Figures 2,3). Despite this growing interest in the field, we found a mean of only 70 citations per article for the top 100 articles. This is probably due to LLR still being a very specialized topic in hepatic surgery with a limited number of authors publishing about it. Also, most of the authors of the 100 top articles are either from France or USA (Table 3), highlighting again that LLR is performed, especially at high volumes, only in a few centers. Nevertheless, all continents are represented with at least one country in the top 100 articles as to show that LLR is spreading around the world.
According to the International Position on LLR, many centers have shown a steady increase in the number of resections each year and publications seem to have followed as a consequence. In the same paper, a consensus of experts proposed the best indications for LLR: a solitary lesion less than 5 cm in diameter and nodules located in the anterior segments (2,4). Technical recommendations included that LLR should be applied far from the hepatic hilum, and the vena cava. Concerning the oncological proficiency with LLR, this should only be adopted if adequate margins can be obtained laparoscopically, keeping a safety distance of the nodule from the line of transection. Six years after the Louisville statement, the Second International Consensus Conference on LLR was held in Morioka, Japan, in 2014 to evaluate the current status of laparoscopic liver surgery and to provide strong recommendations to aid its future development (4). These two consensus conferences have outlined that the indications for LLR are continually expanding. The laparoscopic left lateral sectionectomy is defined as a gold standard procedure (5). Moreover, laparoscopic major hepatectomies are more often proposed as an evolution in the standard of care (6). Even malignancies such as colorectal metastases (7) or HCC (8,9) have been included as standard of care in selected cases. HCC as an indication for LLR is probably the most interesting one and with the greatest potentiality (10). This could explain why seventeen of the top 100 articles on LLR are focused on resections for HCC. LLR for HCC has been shown to improve postoperative morbidity even in patients with Child B cirrhosis (11). Nevertheless, in case of salvage liver transplantation after a laparoscopic resection for HCC, outcomes are comparable to patients who had open surgery including operative time, oncologic radicality, morbidity and mortality, but with the added advantages of laparoscopic surgery such as earlier return to mobility, lower blood losses and less pain (12,13).
Laparoscopic living donor hepatectomy for liver transplantation may encourage both donors and recipients to opt for this type of practice thanks to the reduced invasiveness and higher appeal associated with LLR. However, this procedure is a recognized technical challenge for the surgeon who is probably why we could find only three articles within the top 100 articles on LLR.
Future considerations
Minimally invasive approaches are expected to continue to gain space in liver surgery in the near future. One of the next goals for LLR will be to standardize the practice of resections for HCC in patients with cirrhosis. Surgery for living liver donation remains an extremely challenging field for pure laparoscopic surgery and the aid of robotic assistance could help popularize the adoption of minimally invasive approaches (14).
Conclusions
Having analyzed the 100 top articles on LLR, two main points are to be emphasized: LLR is now performed worldwide and surgical indications are continuing to expand. Furthermore, published articles on LLR are growing proportionally to its widespread. Randomized and prospective studies will be needed to build evidence around this topic and to strengthen the recommendations which to date are mainly based on promising clinical series only.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2017.12.01). GBLS serves as the Editor-in-Chief of Laparoscopic Surgery. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc 1992;6:99.
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Chang S, Laurent A, Tayar C, et al. Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg 2007;94:58-63. [Crossref] [PubMed]
- Dagher I, O'Rourke N, Geller DA, et al. Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg 2009;250:856-60. [Crossref] [PubMed]
- Fuks D, Nomi T, Ogiso S, et al. Laparoscopic two-stage hepatectomy for bilobar colorectal liver metastases. Br J Surg 2015;102:1684-90. [Crossref] [PubMed]
- Goumard C, Komatsu S, Brustia R, et al. Technical feasibility and safety of laparoscopic right hepatectomy for hepatocellular carcinoma following sequential TACE-PVE: a comparative study. Surg Endosc 2017;31:2340-9. [Crossref] [PubMed]
- Levi Sandri GB, Colasanti M, Santoro R, et al. Laparoscopic right hepatectomy for hepatocellular carcinoma in cirrhotic patient. Hepatobiliary Surg Nutr 2015;4:436-8. [PubMed]
- Levi Sandri GB, de Werra E, Mascianà G, et al. Laparoscopic and robotic approach for hepatocellular carcinoma-state of the art. Hepatobiliary Surg Nutr 2016;5:478-84. [Crossref] [PubMed]
- Ettorre GM, Levi Sandri GB. Laparoscopic approach for hepatocellular carcinoma: where is the limit? Chin J Cancer Res 2014;26:222-3. [PubMed]
- Laurent A, Tayar C, Andréoletti M, et al. Laparoscopic liver resection facilitates salvage liver transplantation for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 2009;16:310-4. [Crossref] [PubMed]
- Felli E, Cillo U, Pinna AD, et al. Salvage liver transplantation after laparoscopic resection for hepatocellular carcinoma: a multicenter experience. Updates Surg 2015;67:215-22. [Crossref] [PubMed]
- Levi Sandri GB, de Werra E, Mascianà G, et al. The use of robotic surgery in abdominal organ transplantation: A literature review. Clin Transplant 2017;31. [PubMed]
Cite this article as: Levi Sandri GB, Spoletini G. The one hundred most-cited articles on laparoscopic liver surgery. Ann Clin Oncol 2017;1:3.