
Is elective cholecystectomy effective in geriatric patients to prevent new biliopancreatic events following endoscopic retrograde cholangiopancreatography for benign biliopancreatic pathology?
Highlight box
Key findings
• In aged patients, cholecystectomy is effective in reducing the incidence of acute cholecystitis after endoscopic retrograde cholangiopancreatography (ERCP) procedure for benign biliopancreatic pathology.
• But is associated with a higher risk of post-ERCP choledocholithiasis and acute cholangitis.
What is known and what is new?
• Cholecystectomy is effective in reducing the incidence of acute cholecystitis after ERCP.
• In aged patients, the indication for prophylactic cholecystectomy should not be performed systematically after a benign biliary event requiring ERCP with sphincterotomy, except in cases of previous episodes of acute cholecystitis.
What is the implication, and what should change now?
• In aged and frails patients, prophylactic cholecystectomy should not be indicated systematically.
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a well-established diagnostic and therapeutic endoscopic technique commonly employed for various conditions, and choledocholithiasis is the most frequent benign pathology it addresses (1).
Choledocholithiasis can manifest with a diverse range of symptoms, and ERCP with sphincterotomy (ES) has demonstrated favorable outcomes, even in elderly patients (2-4). Despite the widespread use of this technique and its positive results, studies have linked the performance of ES associated with ERCP to late complications such as cholangitis and pancreatitis, with a variable but typically approximately 10% incidence (5,6).
Biliary duct stones may originate from the gallbladder through the migration of gallstones into the bile duct or can form de novo on the biliary epithelium (7). Recurrent choledocholithiasis is defined as stones reappearing at least 6 months after their prior extraction via ERCP, mostly due to the formation of new stones in the biliary tract caused by duodenal reflux following sphincterotomy (8).
While most patients with gallstones remain asymptomatic throughout their lives, 10% to 25% of them will experience complications, with an annual risk of 2–3% (9). Between 10% and 18% of patients requiring cholecystectomy concurrently have stones in the bile duct (10). The diagnostic confirmation is primarily through imaging studies, and the American Society for Gastrointestinal Endoscopy and the Society of American Gastrointestinal and Endoscopic Surgeons (ASGE-SAGES) has established a probability score for suspected choledocholithiasis: very strong [common bile duct (CBD) stone on ultrasound, bilirubin >4 mg/dL]; strong (CBD >6 mm, bilirubin 1.8–4 mg/dL); and moderate (abnormal liver function tests other than bilirubin, age >55 years, previous acute biliary pancreatitis) (11).
Once the diagnosis is confirmed, preoperative ERCP-ES followed by laparoscopic cholecystectomy (LC) is the most utilized method in clinical practice (9,12).
Elective cholecystectomy is recommended for the treatment of recurrent biliary colic, acute cholecystitis, prevention of pancreatitis, or choledocholithiasis (13). However, there is controversy regarding its efficacy in preventing long-term biliary events after ERCP with sphincterotomy (14). It is known that sphincterotomy does not alter gallbladder function. Moreover, the absence of the gallbladder may hinder effective bile clearance from the bile duct, leading to bile stasis and the formation of larger de novo stones (15). Coupled with the fact that elderly patients develop acute cholecystitis less frequently and the increased risk of lethal events associated with surgery in this age group, there is a need to consider elective cholecystectomy after resolving benign biliary pathology through ERCP-ES in geriatric patients (16).
The aim of this study is to establish the relationship between undergoing ERCP-ES in elderly patients, whether they have had a previous cholecystectomy or not, and the development of medium to long-term biliopancreatic pathology. We present this article in accordance with the STROBE reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-23-19/rc).
Methods
A retrospective study was conducted, analyzing the medical records and imaging studies of patients who underwent ERCP with sphincterotomy (index ERCP) between January 1995 and December 2017. Out of a total of 576 ERCP procedures indicated for benign biliopancreatic pathology, those performed on patients aged 80 years and older were selected, resulting in a cohort of 164 patients. All of them had a minimum follow-up of more than two years, with the aim of avoiding cases with undiagnosed biliopancreatic malignant pathology.
These patients were divided into two groups based on a history of prior cholecystectomy, performed for symptomatic cholelithiasis, before the initial ERCP (index ERCP): Group A [pre-ERCP cholecystectomized (89 patients)] and Group B [noncholecystectomized (75 patients)]. All patients were included with a binomial test to ensure that the groups originated from the same sample in the same proportion (0.5) with a P value of 0.301.
Demographic parameters, medical history, comorbidities, and history of upper digestive tract surgery that could complicate the endoscopic procedure were studied. Parameters related to ERCP were also recorded: indications for ERCP, diagnosis after the procedure, biliary epithelium cytology, stent placement, performance of duodenal precut, diversion from the digestive tube to the bile duct, repetition of ERCP, and reason for repetition.
The only complications studied in this research were the ones that occurred more than 6 months after the index ERCP to avoid including residual choledocholithiasis.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Clinical Trials and Ethics Board of Valladolid University (No. PI 18-889) and individual consent for this retrospective analysis was waived.
Statistical analysis
Statistical analysis was performed using IBM SPSS version 23 software. Statistical significance was defined as P<0.05. The mean, standard deviation (SD), minimum (Min), and maximum (Max) were calculated for all quantitative parameters, while frequency and percentage were used for qualitative parameters. Nonparametric Mann-Whitney U tests were employed to compare the groups, and chi-square and Spearman tests were used for the analysis of the associations among nominal data variables. An independent samples t-test was conducted to analyze the means and correlation of variables of normally distributed data (Kolmogorov-Smirnov normality test, sample size >50) assuming equal variances with Levene’s test for homogeneity of variance.
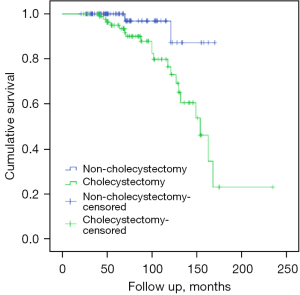
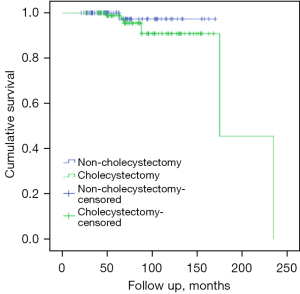
The Kaplan-Meier curve was used to describe the cumulative incidences of choledocholithiasis and cholangitis in the sample. Potential risk factors and benign complications were evaluated through bivariate correlation tests, and Cox logistic regression was applied to explain the hazard ratio (HR) with a P value <0.05 and 95% confidence intervals (95% CIs) using the forward stepwise method of Wald.
Results
The demographic characteristics of the study patients are presented in Table 1.
Table 1
| Characteristics | Group A (N=89) | Group B (N=75) | P value |
|---|---|---|---|
| Sex (men/women) | 29/60 | 31/44 | 0.24 |
| Age, years, median ± SD | 84±3.28 | 86±4.20 | >0.99 |
| Advanced liver disease, n (%) | 1 (1.12) | 4 (5.33) | 0.11 |
| Hypertension, n (%) | 63 (70.79) | 54 (72.00) | 0.86 |
| Diabetes mellitus, n (%) | 16 (17.98) | 18 (24.00) | 0.34 |
| Obesity, n (%) | 11 (12.36) | 7 (9.33) | 0.53 |
| Abuse alcohol intake, n (%) | 5 (5.62) | 5 (6.67) | 0.78 |
| Smoking habit, n (%) | 12 (13.48) | 8 (10.67) | 0.58 |
| Previous foregut surgery, n (%) | 11 (12.36) | 0 | 0.002 |
| Peptic ulcer, n (%) | 14 (15.73) | 10 (13.33) | 0.66 |
| Inflammatory bowel disease, n (%) | 1 (1.12) | 0 | 0.35 |
| Chronic pancreatitis, n (%) | 1 (1.12) | 2 (2.67) | 0.46 |
| Biliary duct dilation, n (%) | 71 (79.78) | 50 (66.67) | 0.058 |
Group A: pre-ERCP cholecystectomy. Group B: without previous cholecystectomy. ERCP, endoscopic retrograde cholangiopancreatography.
Both groups were homogeneous in terms of mean age, sex, and associated comorbidities, with the most frequent comorbidities being hypertension, diabetes mellitus, and smoking habit. The only variable with a statistically significant value was a history of foregut surgery, with 11 procedures in Group A compared to none in Group B (P=0.002) (Table 1).
The mean follow-up was 75 months (range, 21–170 months) for Group A and 89 months (range, 24–235 months) for Group B (without statistically significant). A total of 199 ERCPs were analyzed (164 index, 35 subsequent).
The indications for the index ERCP were quite similar in both groups, except for acute cholangitis, with 20 patients in Group A (22.47%) compared to 12 patients in Group B (16.00%) (P=0.005) (Table 2).
Table 2
| Variables | Group A (N=89) | Group B (N=75) | P value |
|---|---|---|---|
| ERCP indication, n (%) | |||
| Acute pancreatitis | 17 (19.10) | 15 (20.00) | 0.47 |
| Choledocholithiasis | 27 (30.34) | 12 (16.00) | 0.001 |
| Cholestasis/jaundice | 21 (23.60) | 29 (38.67) | 0.02 |
| Cholangitis | 20 (22.47) | 12 (16.00) | 0.005 |
| Biliary leak | 1 (1.12) | 0 | 0.35 |
| Cholecystopancreatitis | 0 | 4 (5.33) | 0.53 |
| Biliary colic | 1 (1.12) | 3 (4.00) | 0.23 |
| Hydatic cyst | 1 (1.12) | 0 | >0.99 |
| others | 1 (1.12) | 0 | 0.35 |
| ERCP diagnosis, n (%) | |||
| Normal biliary duct | 1 (1.12) | 2 (2.67) | 0.85 |
| Choledocholithiasis | 53 (59.55) | 39 (52.00) | 0.008 |
| Biliary sludge | 17 (19.10) | 16 (21.33) | 0.54 |
| Benign stricture | 14 (15.73) | 17 (22.67) | 0.45 |
| Biliary leak | 2 (2.25) | 0 | 0.01 |
| Others | 2 (2.25) | 1 (1.33) | 0.62 |
| Successive ERCP, n (%) | 28 (31.46) | 7 (9.33) | 0.001 |
Group A: pre-ERCP cholecystectomy. Group B: without previous cholecystectomy. ERCP, endoscopic retrograde cholangiopancreatography.
Overall, the most common indication was cholestatic syndrome (50 cases, 30.48%), with 21 patients in Group A (23.60%) vs. 29 patients in Group B (38.67%). Regarding the most common pathology found in the index ERCP, choledocholithiasis topped the list, with 53 patients in Group A (59.55%) compared to 39 patients in Group B (52.00%), showing significant differences (P=0.008) (Table 2).
Biliary duct dilation was documented in 71 patients in Group A (79.78%) vs. 50 patients in Group B (66.67%). Concerning variables related to the procedure, there were no significant differences in stent placement, precut performance, cytology collection, or endoscopic diversion from the bile duct to the digestive tube.
Overall, medium- to long-term biliary events were more frequent in the cholecystectomized group, with 28 (31.46%) compared to 13 (17.33%) in Group B. Except for the incidence of acute pancreatitis, all other complications showed statistically significant differences between the two groups (Table 3).
Table 3
| Variables | Group A (N=89) | Group B (N=75) | P value |
|---|---|---|---|
| Overall complications, n (%) | 28 (31.46) | 13 (17.33) | 0.001 |
| Acute cholecystitis, n (%) | 0 | 10 (13.33) | 0.09 |
| Acute pancreatitis, n (%) | 1 (1.12) | 0 | 0.60 |
| Choledocholithiasis, n (%) | 15 (16.85) | 2 (2.67) | 0.008 |
| Choledocholithiasis successive episodes, n (%) | 5 (5.62) | 0 | |
| Cholangitis, n (%) | 5 (5.62) | 1 (1.33) | 0.03 |
| Cholangitis successive episodes, n (%) | 2 (2.25) | – | |
| Median complications time (months) | 47 | 31 | 0.001 |
| Median choledocholithiasis time (months) | 50 | 31 | 0.003 |
Group A: pre-ERCP cholecystectomy. Group B: without previous cholecystectomy. ERCP, endoscopic retrograde cholangiopancreatography.
Among them, choledocholithiasis was the most common, with a total of 22 cases, 20 in Group A (22.47%) vs. 2 in Group B (2.67%) (P=0.008).
There were also significant differences in the time to onset of the initial complication [47 months in Group A vs. 31 months in Group B (P=0.001)], with recurrent choledocholithiasis occurring at 50 months in Group A vs. 31 months in Group B (P=0.003).
Similarly, in the cholecystectomized group, more ERCPs were repeated [31.46% vs. 9.33% (P=0.001)] (Table 2).
There were 10 cases of acute cholecystitis in group B (13.33%), undergoing surgery. The average time between ERCP and surgery was 8 months.
Kaplan-Meier curves were used to illustrate the survival of patients in the sample (N=164) according to the complications they developed (choledocholithiasis and cholangitis) (Figures 1,2).
The Cox logistic regression method was employed to find a model that predicts or estimates complications in elderly patients regarding the history of cholecystectomy to provide causal-effect relationships and enable individualized decision-making for each patient.
The variables that were included in the predictive model with Wald >6.32, with statistical significance P value <0.012, and that predicted the time of event occurrence (recurrent choledocholithiasis) are as follows: repetition of ERCP, post-ERCP pancreatitis, and ascending cholangitis.
The survival HRs found with the model for the study sample (n=164) are distributed as follows: (I) HR <1, number of patients: 29; (II) HR >1, number of patients: 8; and (III) HR =1, number of patients: 127. According to the above results, overall, repetition of ERCP does not affect survival after choledocholithiasis events.
The model is suitable with a global chi-square =77.96 and P<0.001. This ensures that the model fits the data perfectly as the likelihood differs from 1. The model predicts a large percentage of events in the sample (n=164).
Discussion
In general, prophylactic cholecystectomy following ERCP-ES for benign biliopancreatic pathology is considered to reduce the subsequent incidence of biliary and pancreatic events (17-19). However, this therapeutic approach in elderly patients remains a topic of ongoing debate (17). Additionally, it has been observed that cholecystectomy in patients with a history of choledocholithiasis treated by ERCP with ES is associated with higher complexity, conversion rates, morbidity, and associated complications (20,21).
Furthermore, the prevalence of cholecystectomy after ERCP for choledocholithiasis is only 22% and 8% in patients aged ≥75 years and ≥85 years, respectively. The main reason for this could be the comorbidity burden or frailty of elderly patients, likely due to the comorbidities and frailty associated with advanced age (22).
Nevertheless, based on the risk of complications when deferring post-ERCP cholecystectomy, some authors recommend an active approach even in this patient population if there are no absolute contraindications to anesthesia or surgery (17). This study, a meta-analysis with a large number of cases, finds that prophylactic cholecystectomy reduces the incidence of acute cholecystitis, cholangitis, pancreatitis and biliary events after ERCP. However, the average age of the included data series ranges between 48–85 years and only one of them has an average age greater than 80 years.
Various risk factors related to the development of biliary complications after ERCP have been identified, such as the presence of large stones, the use of lithotripsy, and bile duct dilation (23,24). In our cohort, although bile duct dilation was observed in 73.78% of the index ERCPs, this variable was not identified as a risk factor associated with increased complications.
Overall, the incidence of medium/long-term complications after ERCP is approximately 10% (5,25). Sousa et al., in a retrospective study of 131 patients with a mean age of 82 years, found a post-ERCP complication rate of 13%. Fewer biliary events were reported in patients who had a cholecystectomy (7% vs. 24%) (22). In our cohort, we found an overall incidence of post-ERCP complications of 18.29%, which was higher in the previously cholecystectomized group (30.33% vs. 4%). Therefore, in our model, prior cholecystectomy was associated with a higher incidence of post-ERCP biliary events.
The most frequent complication found was recurrent choledocholithiasis followed by ascending cholangitis. While repetition of ERCP was effective and did not increase the mortality in our series for that reason. Kanamori et al. (26) presented a cohort of 250 patients over 80 years old, and they analyzed, among other factors, the performance of cholecystectomy, and concluding that it prevented the recurrence of subsequent complications such as cholangitis, choledocholithiasis, and pancreatitis. However, their analysis was global, and they did not compare age groups. The same is true in the meta-analysis conducted by Mc Geehan (17), where only one of the included series grouped patients over 80 years old.
On the other hand, Heo et al. (27) designed a prospective study in patients who underwent ERCP for choledocholithiasis and randomized them for prophylactic cholecystectomy. In their conclusions, cholecystectomy logically reduced the risk of cholecystitis but not the risk of recurrent cholangitis. The same result was found by Song et al. for the recurrence of choledocholithiasis in a case-control study (28). Our data confirm these findings.
Yasui et al. (15) followed a cohort of 327 patients for 10 years, with 77 over 80 years old, and concluded that they do not recommend intervening after ERCP in patients over 80 years old. The overall biliary complications were significantly lower in cholecystectomized patients than in patients with the gallbladder in situ in the young group (7.5% vs. 21.7%, P=0.0037), but not different in the elderly group, like the findings in our study, which also has a longer follow-up range.
Cui et al.’s study (29) did not differentiate between age groups, presented 164 noncholecystectomized patients, of which only 44 were found to have gallstones. They concluded that prophylactic cholecystectomy should only be recommended in patients with gallstones due to the high risk of developing cholecystitis and that prophylactic cholecystectomy could not be recommended for all patients after ERCP.
Interestingly, in our cohort, although the number of post-ERCP complications are higher in cholecystectomized patients, the complications occurred later in this group of patients than in noncholecystectomized patients.
Limits of the study
A limitation of our study is its retrospective nature, so the pre-ERCP cholecystectomy group was not randomized, and for this reason, there may be selection and analysis biases. Additionally, data were collected from the patients who survived, and the follow-up was continued for at least 2 years after ERCP, so any serious complications after surgery may not be fully reflected.
Our data are based on a cohort of patients treated at our center but reflect the demographics of elderly patients in our setting. Obviously, a larger sample size would allow better generalization of the results.
Conclusions
In conclusion, based on the data from this study, patients over 80 years old who have undergone a previous cholecystectomy present higher benign biliary complication after an initial episode requiring ERCP with associated sphincterotomy than those who have not undergone cholecystectomy. Therefore, we believe that the indication for prophylactic cholecystectomy in this group of patients should not be performed routinely following a benign biliary event requiring ERCP with sphincterotomy. Patients with a history of upper digestive tract surgery and acute cholecystitis may benefit from prophylactic cholecystectomy, while a “watch and wait” approach could be a good option for others.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-23-19/rc
Data Sharing Statement: Available at https://ls.amegroups.com/article/view/10.21037/ls-23-19/dss
Peer Review File: Available at https://ls.amegroups.com/article/view/10.21037/ls-23-19/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-23-19/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Clinical Trials and Ethics Board of Valladolid University (No. PI 18-889) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- ASGE Standards of Practice Committee. The role of ERCP in benign diseases of the biliary tract. Gastrointest Endosc 2015;81:795-803. [Crossref] [PubMed]
- ASGE Standards of Practice Committee. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc 2019;89:1075-1105.e15. [Crossref] [PubMed]
- Saito H, Koga T, Sakaguchi M, et al. Safety and Efficacy of Endoscopic Removal of Common Bile Duct Stones in Elderly Patients ≥90 Years of Age. Intern Med 2019;58:2125-32. [Crossref] [PubMed]
- Bass GA, Gillis AE, Cao Y, et al. Patients over 65 years with Acute Complicated Calculous Biliary Disease are Treated Differently-Results and Insights from the ESTES Snapshot Audit. World J Surg 2021;45:2046-55. [Crossref] [PubMed]
- Langerth A, Brandt L, Ekbom A, et al. Late Complications following Endoscopic Sphincterotomy for Choledocholithiasis: A Swedish Population-Based Study. Diagn Ther Endosc 2014;2014:745790. [Crossref] [PubMed]
- Fujimoto T, Tsuyuguchi T, Sakai Y, et al. Long-term outcome of endoscopic papillotomy for choledocholithiasis with cholecystolithiasis. Dig Endosc 2010;22:95-100. [Crossref] [PubMed]
- Peñas-Herrero I, de la Serna-Higuera C, Perez-Miranda M. Endoscopic ultrasound-guided gallbladder drainage for the management of acute cholecystitis (with video). J Hepatobiliary Pancreat Sci 2015;22:35-43. [Crossref] [PubMed]
- Oliveira-Cunha M, Dennison AR, Garcea G. Late Complications After Endoscopic Sphincterotomy. Surg Laparosc Endosc Percutan Tech 2016;26:1-5. [Crossref] [PubMed]
- Pavlidis ET, Pavlidis TE. Current management of concomitant cholelithiasis and common bile duct stones. World J Gastrointest Surg 2023;15:169-76. [Crossref] [PubMed]
- Moreira Vicente VF, Meroño García E, López San Román A, et al. Coledocolitiasis en pacientes no colecistectomizados: esfinterotomía endoscópica y después colecistectomía? Rev Esp Enferm Dig 1989;76:215-21.
- Tracy BM, Poulose BK, Paterson CW, et al. National adherence to the ASGE-SAGES guidelines for managing suspected choledocholithiasis: An EAST multicenter study. J Trauma Acute Care Surg 2022;92:305-12. [Crossref] [PubMed]
- Jorba R, Pavel MC, Llàcer-Millán E, et al. Contemporary management of concomitant gallstones and common bile duct stones: a survey of Spanish surgeons. Surg Endosc 2021;35:5024-33. [Crossref] [PubMed]
- Dasari BV, Tan CJ, Gurusamy KS, et al. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 2013;2013:CD003327. [PubMed]
- Ando T, Tsuyuguchi T, Okugawa T, et al. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut 2003;52:116-21. [Crossref] [PubMed]
- Yasui T, Takahata S, Kono H, et al. Is cholecystectomy necessary after endoscopic treatment of bile duct stones in patients older than 80 years of age? J Gastroenterol 2012;47:65-70. [Crossref] [PubMed]
- Hui CK, Lai KC, Yuen MF, et al. Role of cholecystectomy in preventing recurrent cholangitis. Gastrointest Endosc 2002;56:55-60. [Crossref] [PubMed]
- Mc Geehan G, Melly C, O' Connor N, et al. Prophylactic cholecystectomy offers best outcomes following ERCP clearance of common bile duct stones: a meta-analysis. Eur J Trauma Emerg Surg 2023;49:2257-67. [Crossref] [PubMed]
- McCarty TR, Farrelly J, Njei B, et al. Role of Prophylactic Cholecystectomy After Endoscopic Sphincterotomy for Biliary Stone Disease: A Systematic Review and Meta-analysis. Ann Surg 2021;273:667-75. [Crossref] [PubMed]
- Boerma D, Rauws EA, Keulemans YC, et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet 2002;360:761-5. [Crossref] [PubMed]
- Lee JM, Chung WC, Sung HJ, et al. Factor analysis of recurrent biliary events in long-term follow up of gallstone pancreatitis. J Dig Dis 2017;18:40-6. [Crossref] [PubMed]
- Kuy S, Sosa JA, Roman SA, et al. Age matters: a study of clinical and economic outcomes following cholecystectomy in elderly Americans. Am J Surg 2011;201:789-96. [Crossref] [PubMed]
- Sousa M, Pinho R, Proença L, et al. Choledocholithiasis in elderly patients with gallbladder in situ - is ERCP sufficient? Scand J Gastroenterol 2018;53:1388-92. [Crossref] [PubMed]
- Paspatis GA, Paraskeva K, Vardas E, et al. Long-term recurrence of bile duct stones after endoscopic papillary large balloon dilation with sphincterotomy: 4-year extended follow-up of a randomized trial. Surg Endosc 2017;31:650-5. [Crossref] [PubMed]
- Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol 2002;97:2763-7. [Crossref] [PubMed]
- Sugiyama M, Suzuki Y, Abe N, et al. Endoscopic retreatment of recurrent choledocholithiasis after sphincterotomy. Gut 2004;53:1856-9. [Crossref] [PubMed]
- Kanamori A, Kiriyama S, Tanikawa M, et al. Long- and short-term outcomes of ERCP for bile duct stones in patients over 80 years old compared to younger patients: a propensity score analysis. Endosc Int Open 2016;4:E83-90. [PubMed]
- Heo J, Jung MK, Cho CM. Should prophylactic cholecystectomy be performed in patients with concomitant gallstones after endoscopic sphincterotomy for bile duct stones? Surg Endosc 2015;29:1574-9. [Crossref] [PubMed]
- Song ME, Chung MJ, Lee DJ, et al. Cholecystectomy for Prevention of Recurrence after Endoscopic Clearance of Bile Duct Stones in Korea. Yonsei Med J 2016;57:132-7. [Crossref] [PubMed]
- Cui ML, Cho JH, Kim TN. Long-term follow-up study of gallbladder in situ after endoscopic common duct stone removal in Korean patients. Surg Endosc 2013;27:1711-6. [Crossref] [PubMed]
Cite this article as: Martín-del Olmo JC, Gómez-López JR, Concejo-Cutoli P, Trujillo-Díaz JC, Vaquero-Puerta C, Ibáñez-García M. Is elective cholecystectomy effective in geriatric patients to prevent new biliopancreatic events following endoscopic retrograde cholangiopancreatography for benign biliopancreatic pathology? Laparosc Surg 2024;8:2.


